blog
Provider Data Management with Sanator: All You Need to Know
SECTIONS
In January this year, the No Surprises Act – part of the Consolidated Appropriations Act of 2021 – went into effect, requiring US health plans to verify and update their provider directories within 48 hours of changes to provider information. Legislators expect the implementation of this act will alleviate the financial burden of unexpected medical billings due to inadvertent out-of-network services – which happen approximately 20%Opens in a new tab of the time in emergency room visits and as much as 16% of non-emergency hospitalizations. For healthcare organizations that will now absorb any costs associated with surprise billings, the act has created a sense of urgency regarding provider data management in healthcare.
With health plans and providers scrambling for new solutions to the challenges of timely provider data management, healthcare organizations should audit the state of their data management processes to identify any systemic shortcomings. In this guide, you’ll learn what provider data management is and its challenges to the healthcare industry.
Key Takeaways:
- The No Surprises Act has added urgency to the existing difficulties of provider data management.
- Provider data management involves collecting and maintaining comprehensive and accurate records of contact and service information for healthcare providers associated with an organization.
- Lack of data collection and quality standardization creates persistent challenges in provider data management.
What Is Provider Data Management?
In healthcare, provider data refers to the information organizations collect and maintain to connect patients with the healthcare professionals and services they need. These connections may include referrals to specialists, license providers, exchange information, labs and medical imaging, and dozens of other services patients routinely require.
Who Is a Provider?
While organizations may have had a simpler definition of who exactly a provider is in the past, changes in the practice and distribution of healthcare services in the last decade have complicated that definition. In addition to traditional healthcare service providers, such as hospitals, clinics, and private practices, a contemporary organization’s provider data would also comprise:
- Nurse practitioners
- Social workers
- Substance abuse counselors
- Behavioral science organizations
- Community health centers and other community-based organizations
The expanded sense of providers in healthcare contexts tracks with the industry shift towards value-based care that incorporates social determinants of health such as patients’ housing situations, transportation, employment, and access to healthy food.
What Is Provider Data?
For all providers, a dataset should exist in the databases of all associated organizations and institutions with whom they interact in healthcare operations. In most instances – for individual providers, groups, and institutions, provider data would consist of:
- Names of individuals or organizations
- Contact information such as phone numbers, email, websites, and self-service portals
- Associated health plans and networks
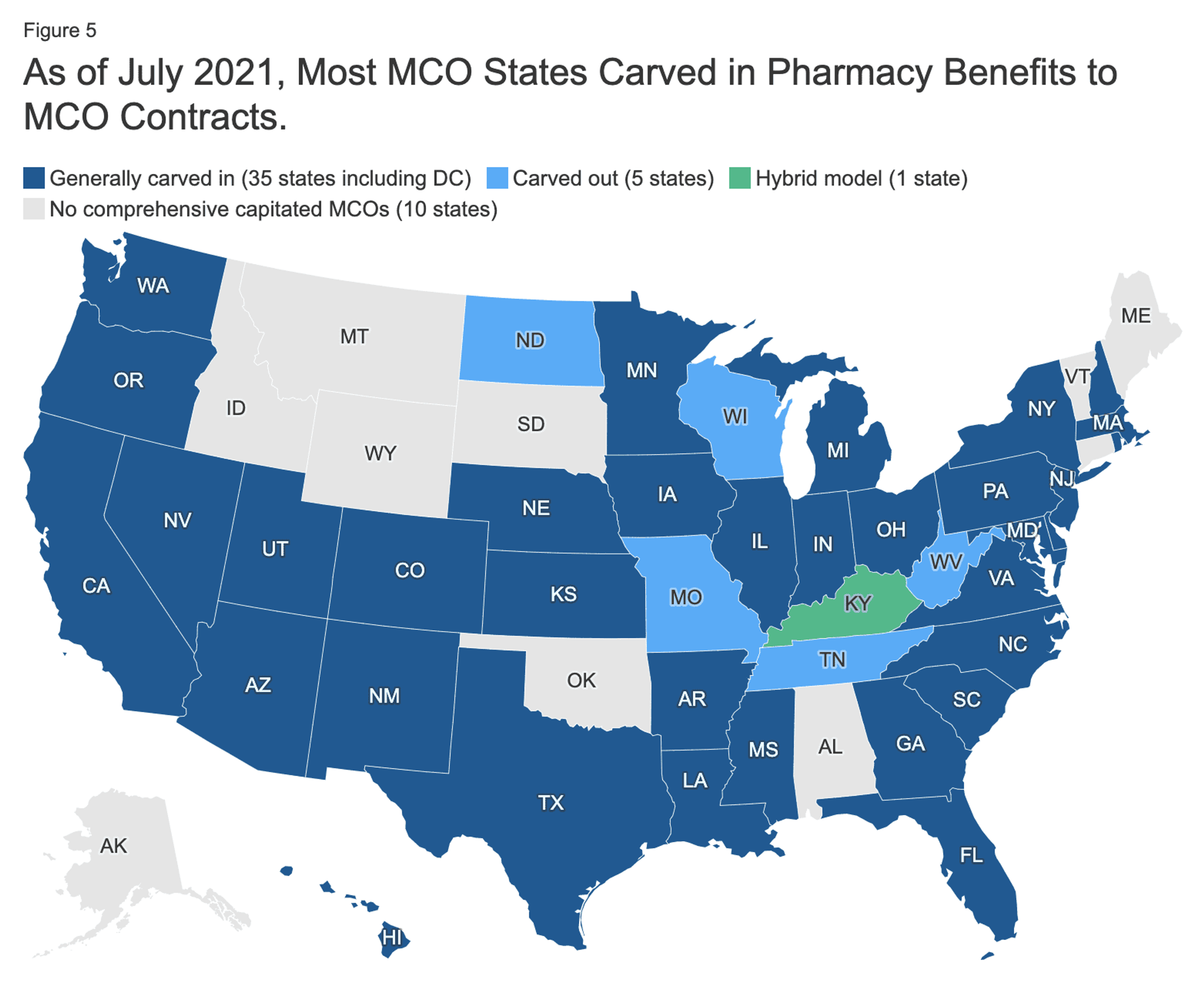
Image Source: kff.org
While maintaining current provider contact and service databases may seem relatively straightforward, standardizing it has proven challenging. Individual practices may hold more than a dozen managed care contracts with health plans, each representing 140Opens in a new tab different provider data elements. Recent trendsOpens in a new tab in most states to carve in behavioral health, pharmacy, dental, and long-term services and supports to managed care organizations will further compound this complexity.
Why Is Provider Data Important?
Gaps or inaccuracies in provider data cause wasted time and resources, generating surprise medical charges, and ultimately resulting in a lower overall standard of care delivered to patients. Common, avoidable problems caused by poor provider data include:
- Patients seeking care from out-of-network providers
- Billing and administrative complications for providers
- Health plans risk violations of state and federal requirements, which bloats administrative burdens and costs in the long run
3 Persistent Challenges in Provider Data Management
Here are three challenges healthcare organizations face in collecting and maintaining comprehensive and accurate provider data.
1. Lack of Standardized Data Collection Methods
Because the healthcare industry lacks a standard method for obtaining and managing provider data – a single source of truth – every organization must decide how best to acquire and import data into their systems. This often leads to patchwork ad hoc methods involving disproportionate amounts of manual time and effort sourcing, extracting, and loading data.
Additionally, when organizations concoct their own data management methods, they apply differing validations, complicating the efficient data exchange between systems and organizations.
2. Lack of Standardized Definitions for Data Quality
In any industry, data quality and integrity generally refer to how usable data is for specified purposes in the state it originates. It has low quality if a given amount of data requires a significant amount of time and energy to process and cleanse before it can serve a useful purpose. It has high quality if users can take it as is and accomplish specified tasks.

Image Source: smartbridge.com
Although some subjectivity in the process is inevitable, organizations in many industries and fields use a six-domain modelOpens in a new tab to assess data quality. These domains are:
- Accuracy
- Completeness
- Consistency
- Timeliness
- Processability
- Accessibility
Currently, the healthcare industry lacks consensus on minimum standards for provider data quality. This results in significant quality gaps between providers, such as health plan provider networks and marketing materials distributed to potential providers. Because these gaps often exist between different iterations of the same data, organizations unknowingly make costly and redundant investments in cleaning up the same data.
3. Lack of Means for Data Producers to Hold Each Other Accountable
While limited federal and state regulatory requirements apply to provider data quality in health plans, enforcement remains inconsistent and generally non-applicable to other providers. Data science is relatively new to most industries, but the more organizations apply it, the more they find unanticipated systemic faults. In large organizations and enterprises – those with the IT resources to practice data managementOpens in a new tab – bad data is surprisingly endemic, accounting for as much as 40%Opens in a new tab of the whole. Without better regulatory controls, the burden of developing and maintaining standards falls on individual organizations.
Provider Network Data Management with Sanator by Gaine
Designed specifically for the unique challenges of healthcare data management, Coperor by Gaine seamlessly integrates data across organizations and contracted partners to create a single source of truth in your organization. With Sanator, you can create, exchange, and apply data in all provider network data management operations with the highest confidence.
To schedule a live demo, contact Gaine today.
