How Data Stewardship Protects Healthcare Organizations
Discover how strong data stewardship protects your organization from compliance gaps, security threats, and operational inefficiencies.
Gain(e) a clear, unified view of your claims data, identify and resolve issues proactively, and improve collaboration with payers.
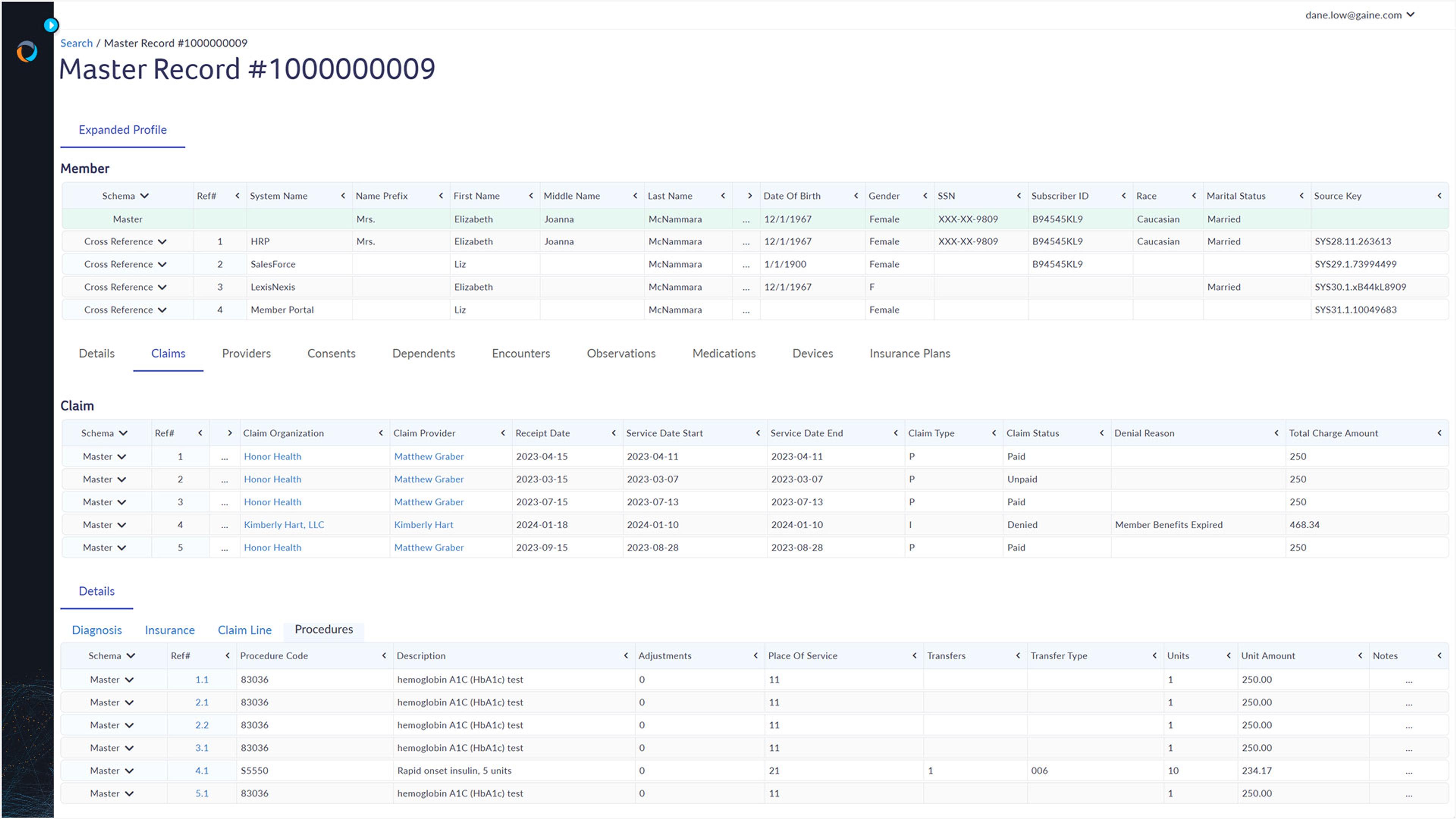
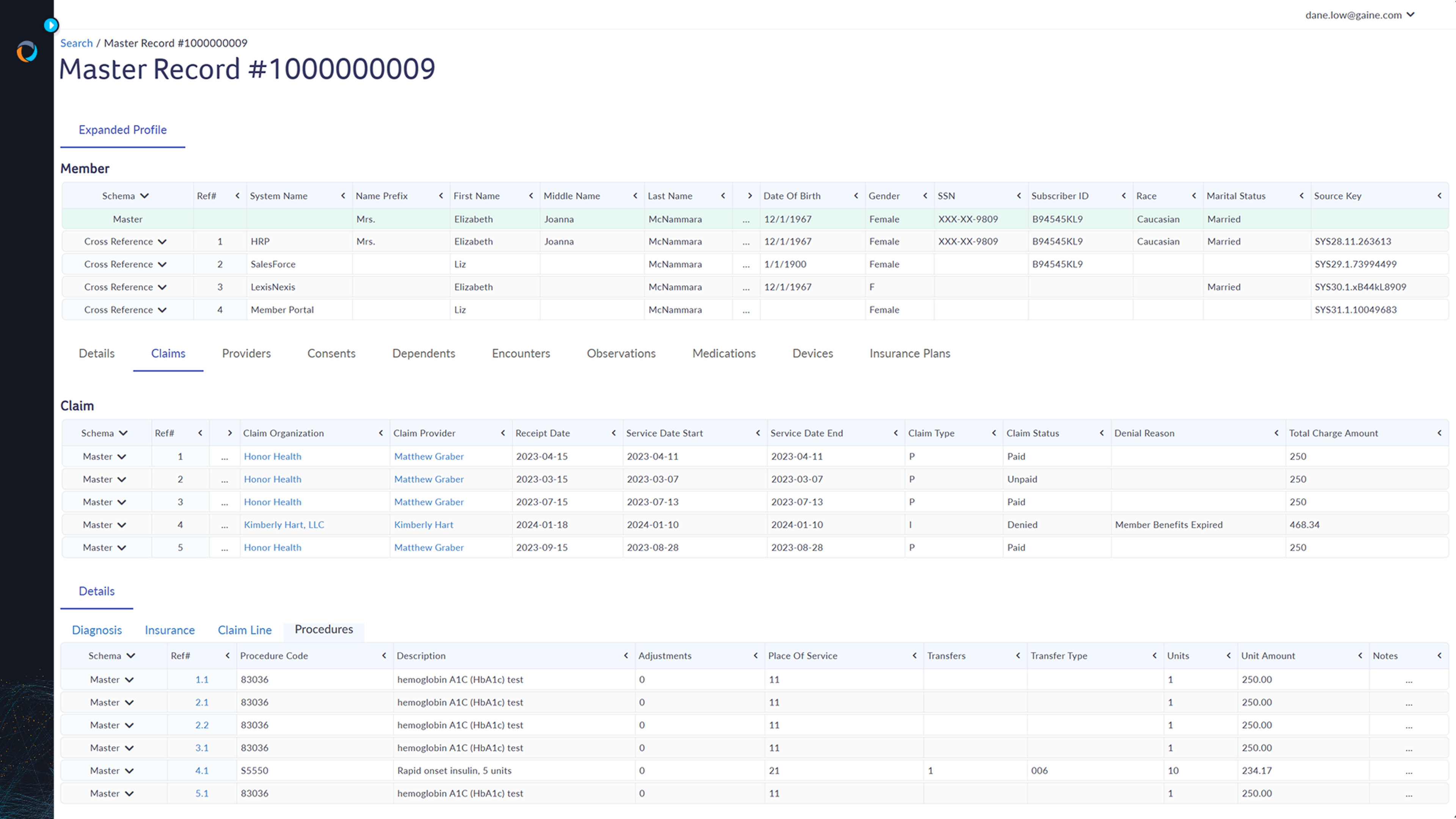
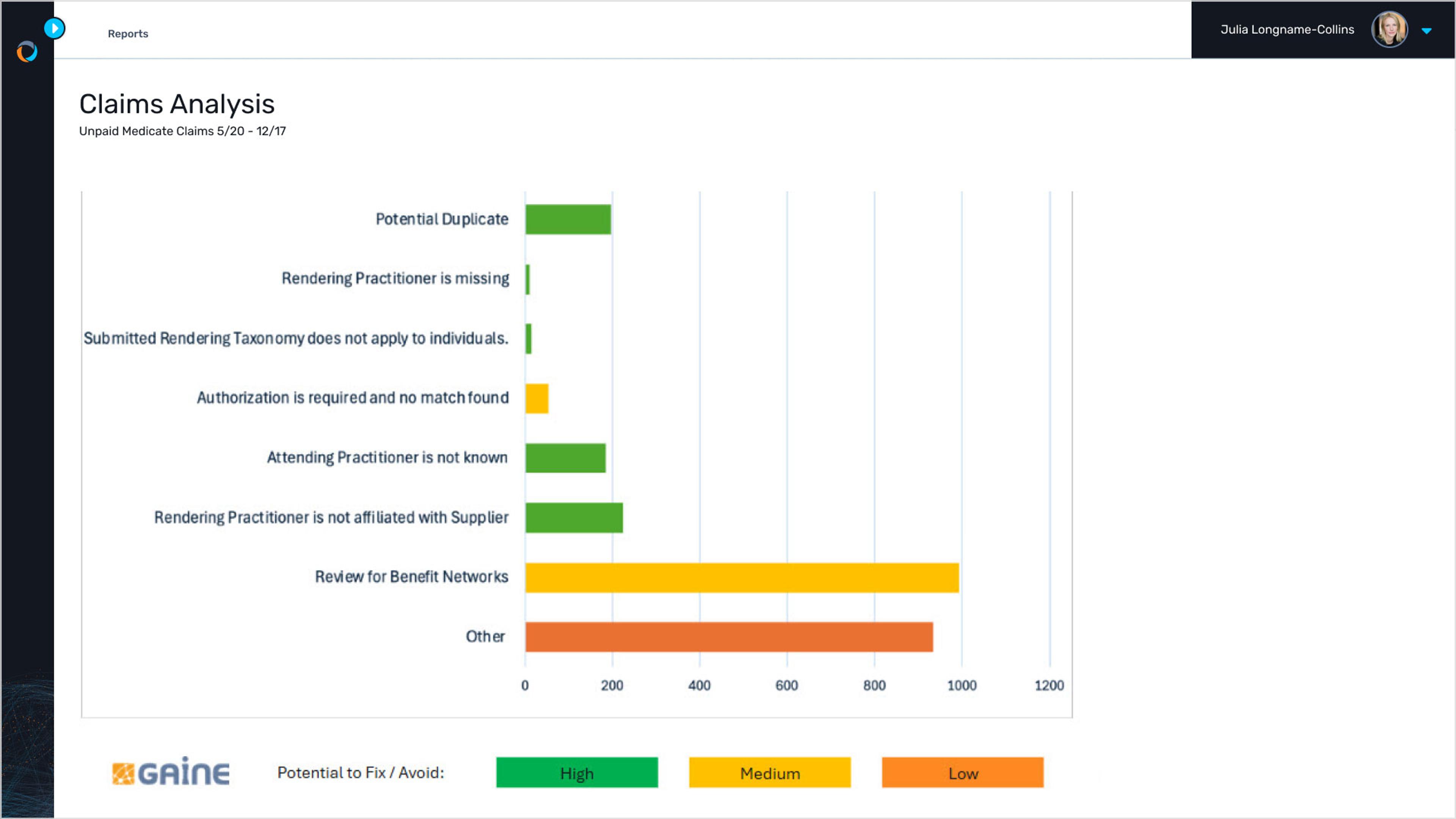
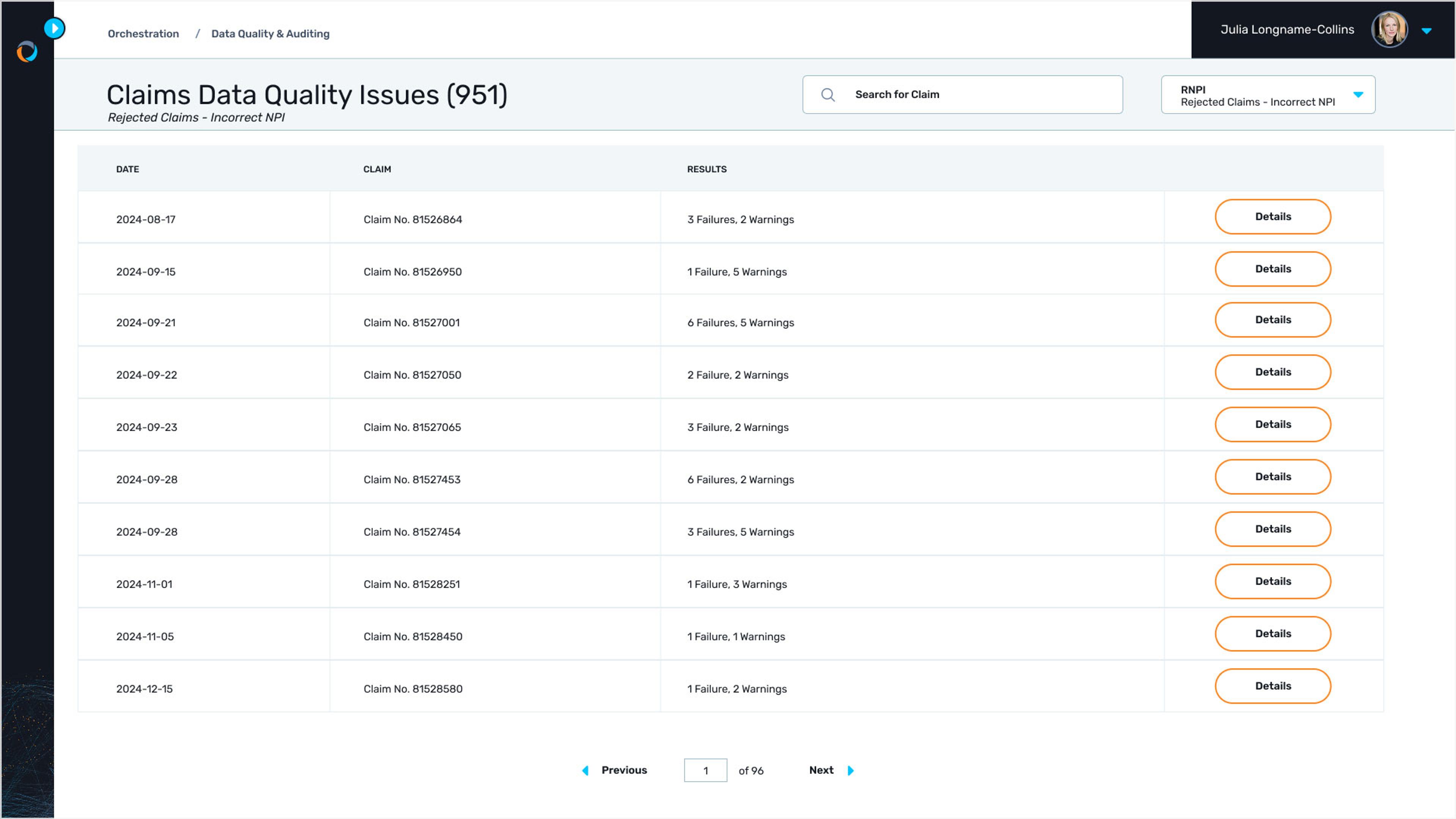
Denied or delayed claims significantly impact a provider group’s revenue cycle and financial stability. Take control of your claims process. Create a unified view of claims data, using advanced analytics to quickly identify root causes for claims denials. Because you’re using technology, you can use a proactive strategy to resolve issues before they happen, improve payer collaboration, and make data-driven decisions (but really this time) for a more efficient and effective claims management process.
CEO of Small Provider Group in AK
Bring together all your claims data, no matter where it’s coming from, into a single, unified view. Integrate with your existing claims systems, EHRs, and other sources to create a comprehensive and up-to-the-minute picture of your claims activity.
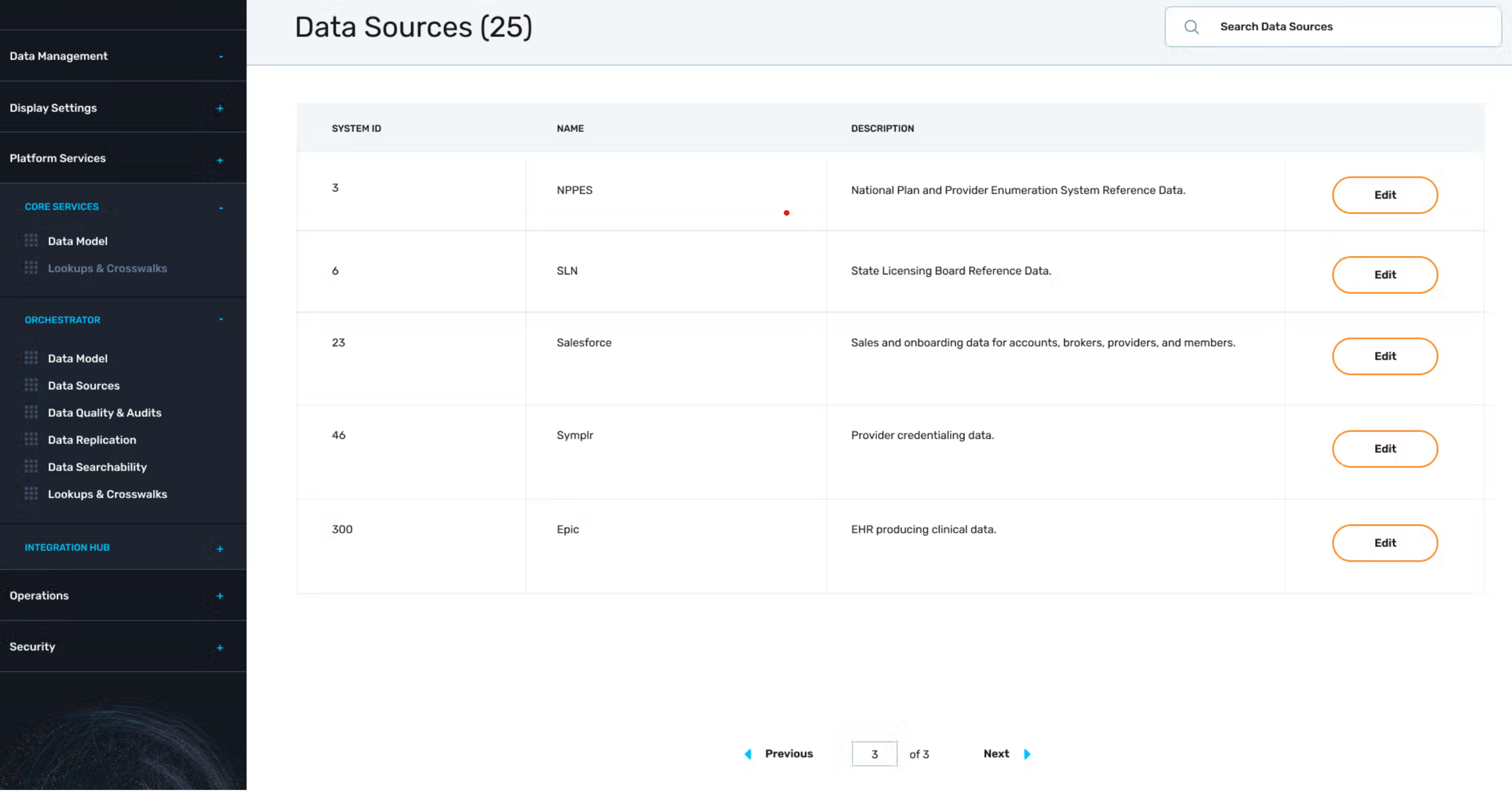
Connect with any system
Seamlessly integrate Gaine with your existing claims management systems, EHRs, contracting and credentialling systems, and other healthcare applications.
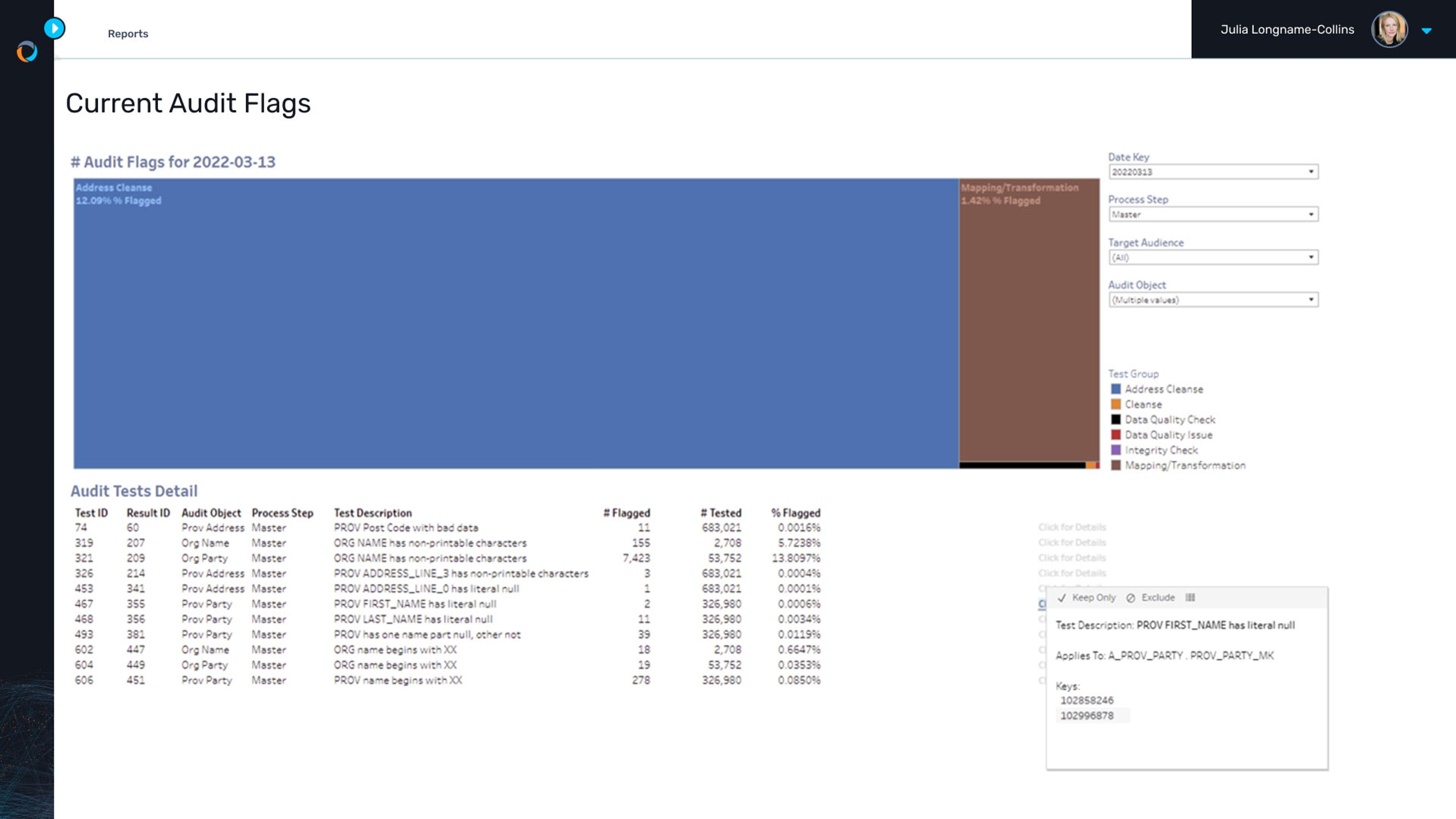
Ensure data accuracy
Gaine’s data quality tools automatically identify and resolve errors, inconsistencies, and duplicates in claims data, as well as related data like providers, service locations, affiliations, and more.
Unlock data insights
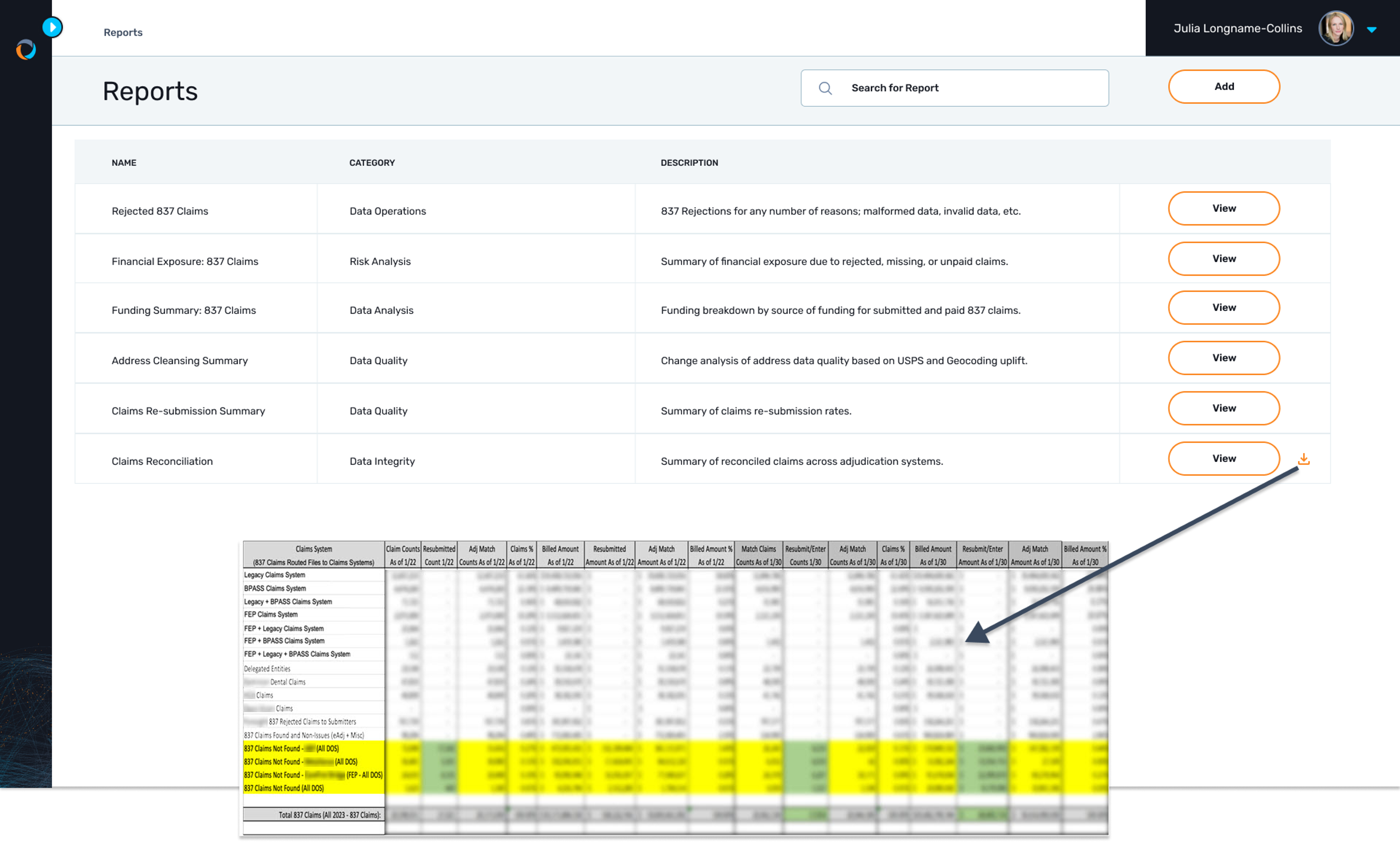
Utilize Gaine's advanced analytics and reporting tools to Gain(e) insights into claim trends, cost drivers, and payer performance.
Slash denials and revenue loss
Proactively prevent claims denials and revenue loss through data validation, error correction, and automated software.
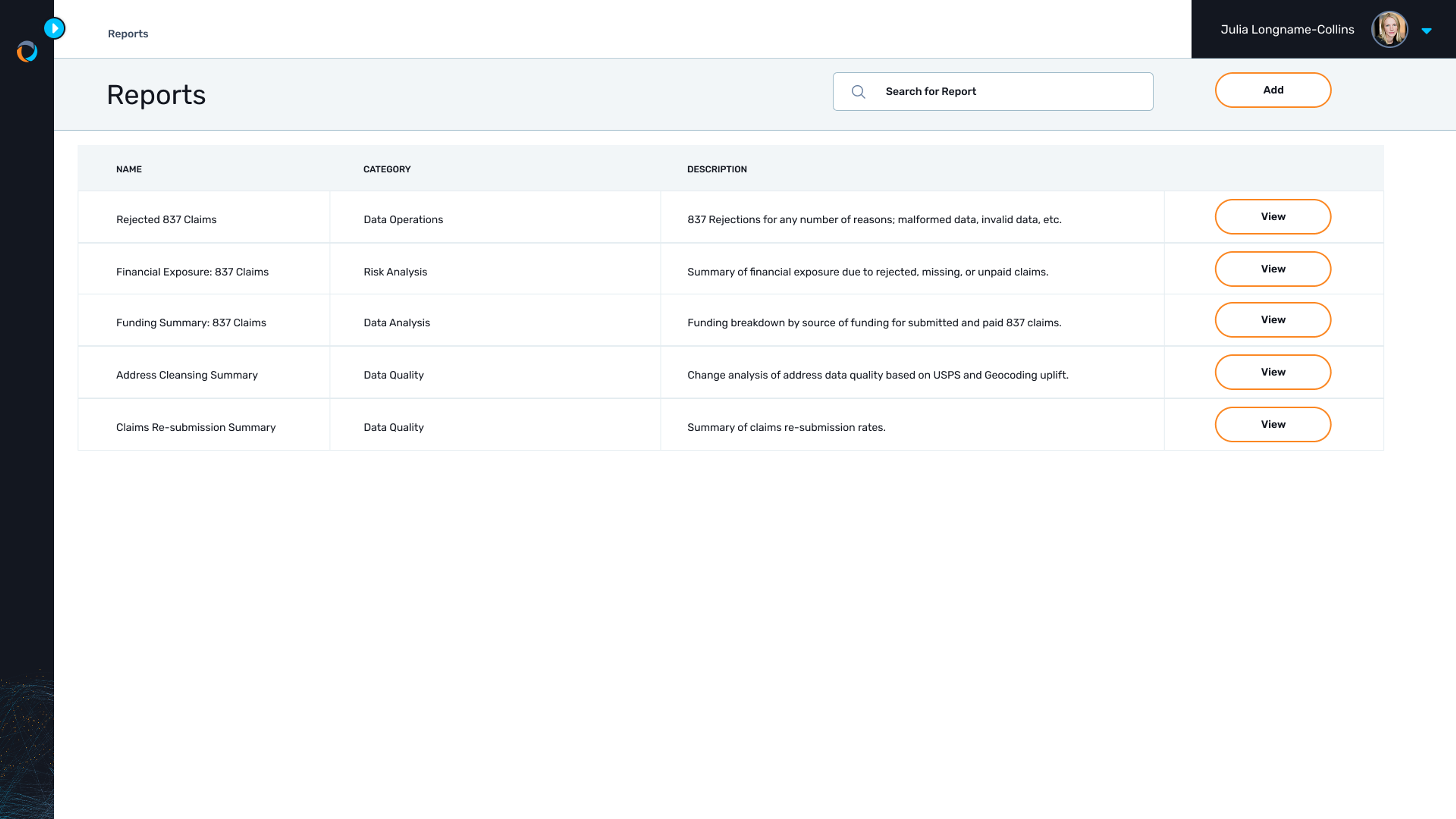
Generate custom reports
Create custom reports tailored to your specific needs, providing valuable insights into claims performance and trends. Our services team does this for you.
Share and collaborate with payers
Securely share claims data with payers to facilitate collaboration, resolve discrepancies, and improve payment processes.