CLAIMS DATA MANAGEMENT – PAYERS
Take control of your claims data and transform your claims management process
Unify, cleanse, and analyze your claims data, unlocking valuable insights and driving better decision-making.
OVERVIEW
Optimize your claims management
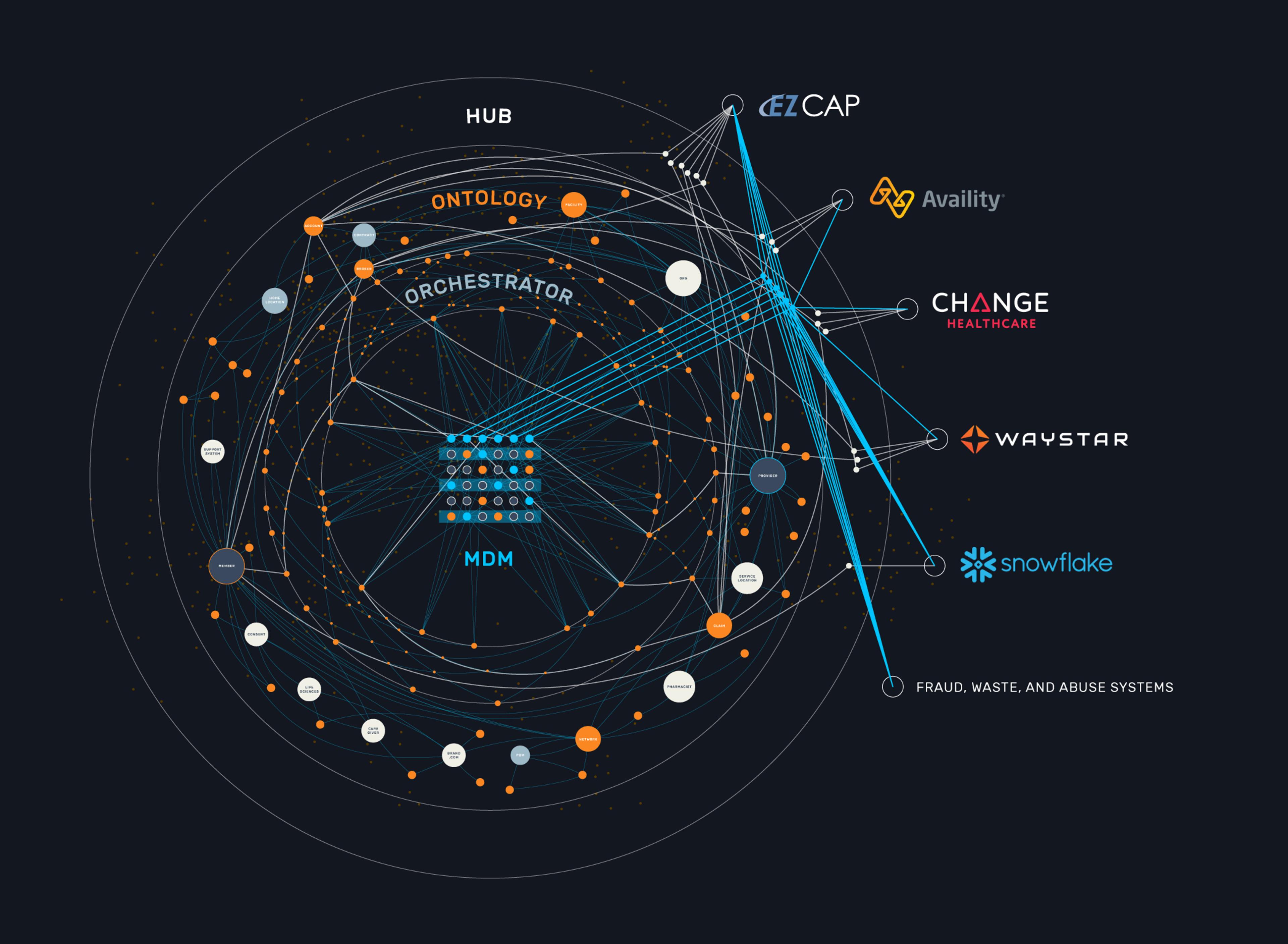
Payers face mounting pressure to control costs, improve efficiency, and enhance the member experience. Gaine's Claims Data Management solution empowers payers to overcome these challenges by providing a unified view of claims data, advanced analytics, and streamlined workflows. Proactively identify issues, improve provider collaboration, and make (actual) data-driven decisions for a more efficient and effective claims management process.
Why Gaine claims data management (for Payers)
Consolidate claims data
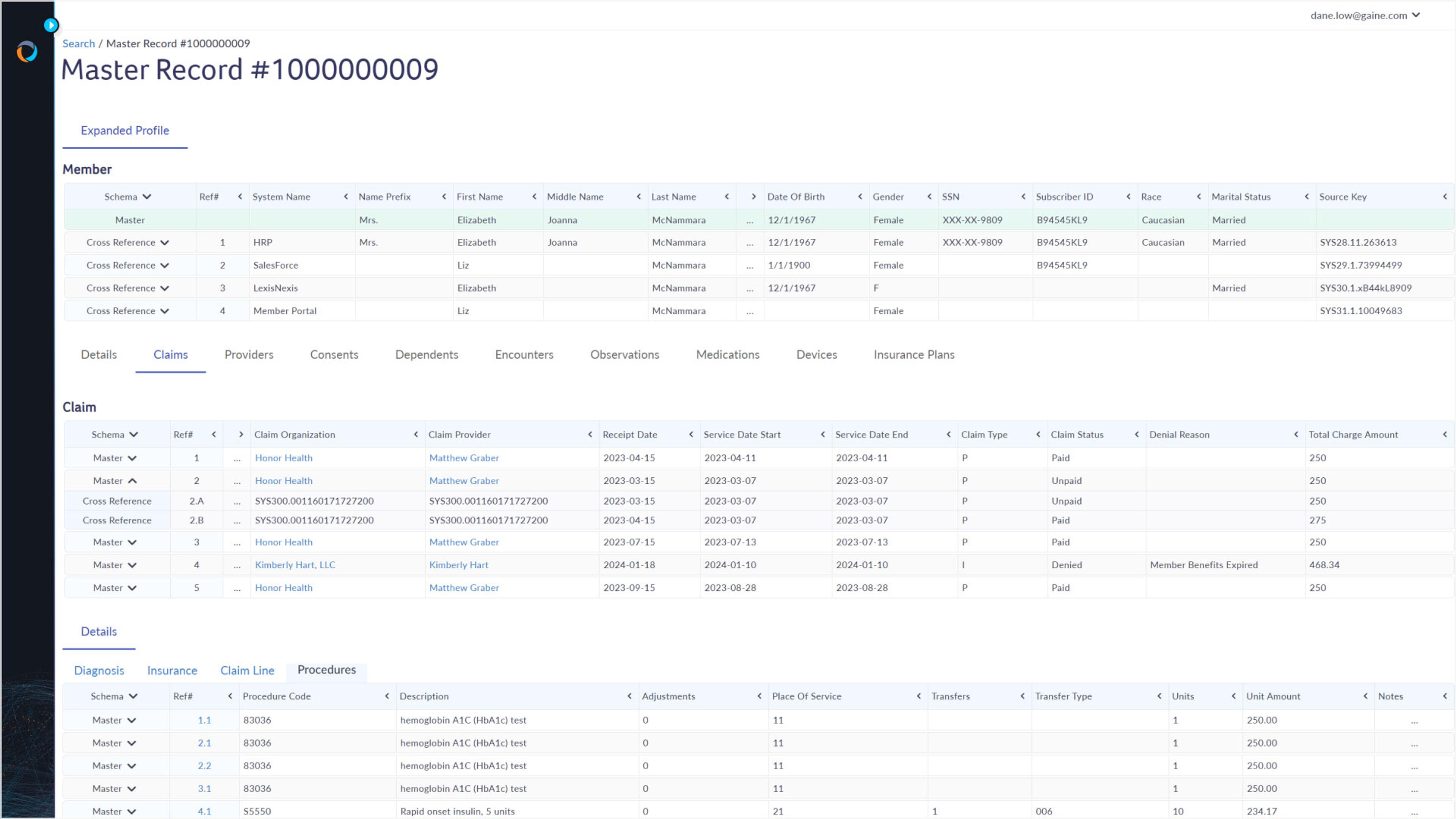
Integrate claims data with various sources, including member information, provider data, and clinical data, creating a unified view for comprehensive analysis and reconciliation. You’ll Gain(e) a holistic understanding of your claims data, identify trends and patterns, and make more informed decisions. By combining claims data with other relevant information in real-time, you can identify potential issues and opportunities for improvement.
Feature highlights
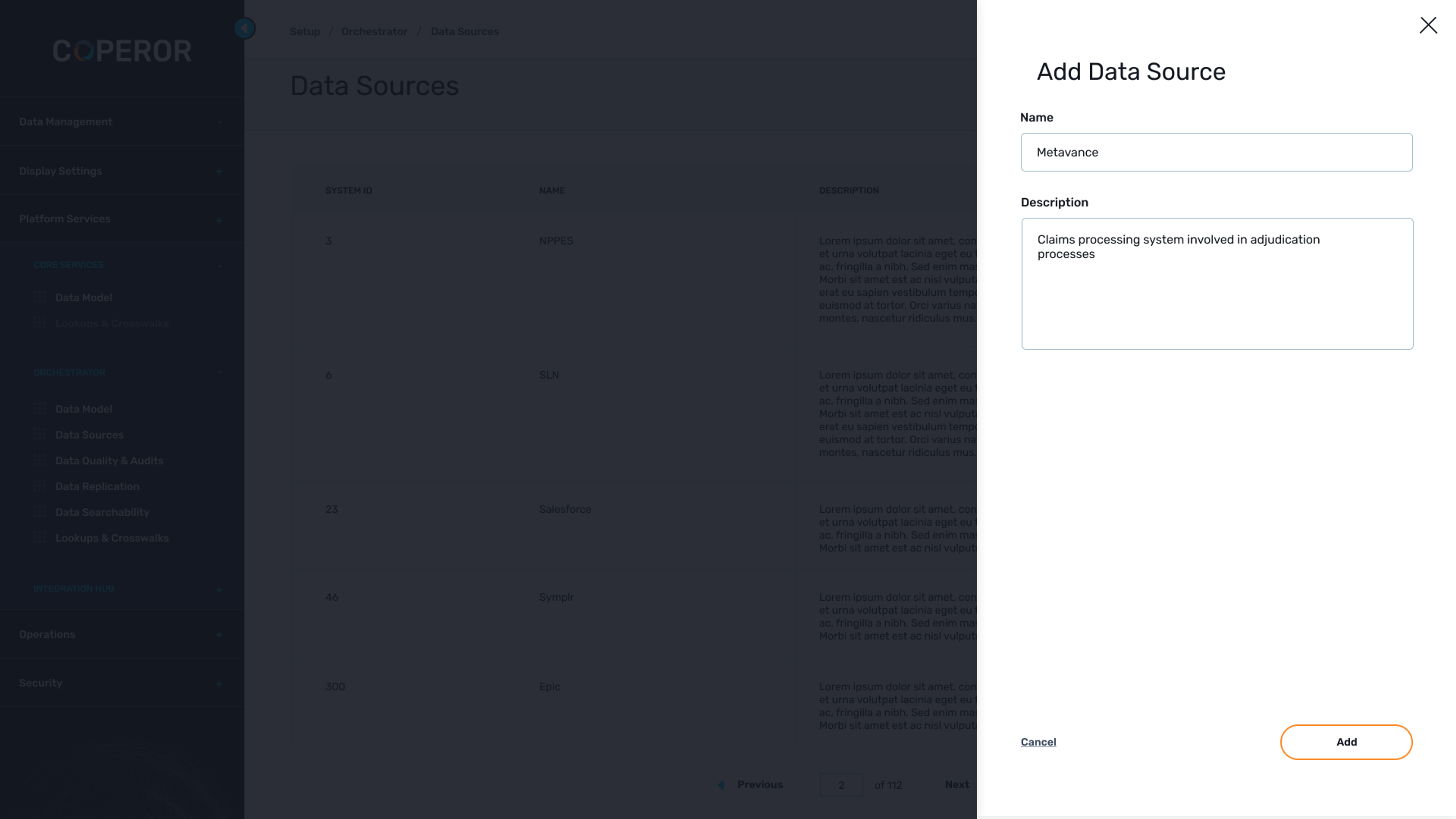
Connect with any system
Seamlessly integrate Gaine with your existing claims management systems, data warehouses, and other healthcare applications.
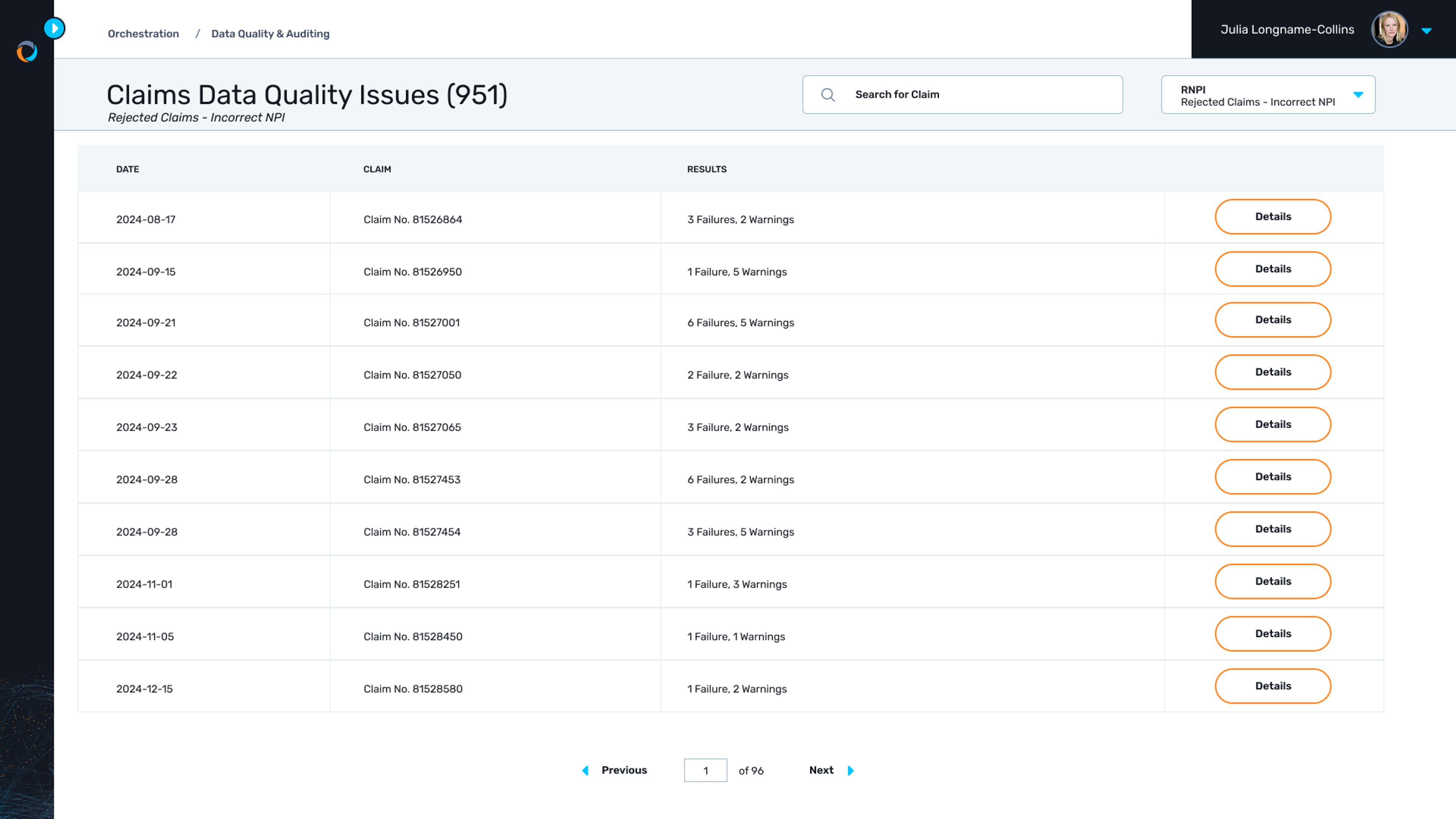
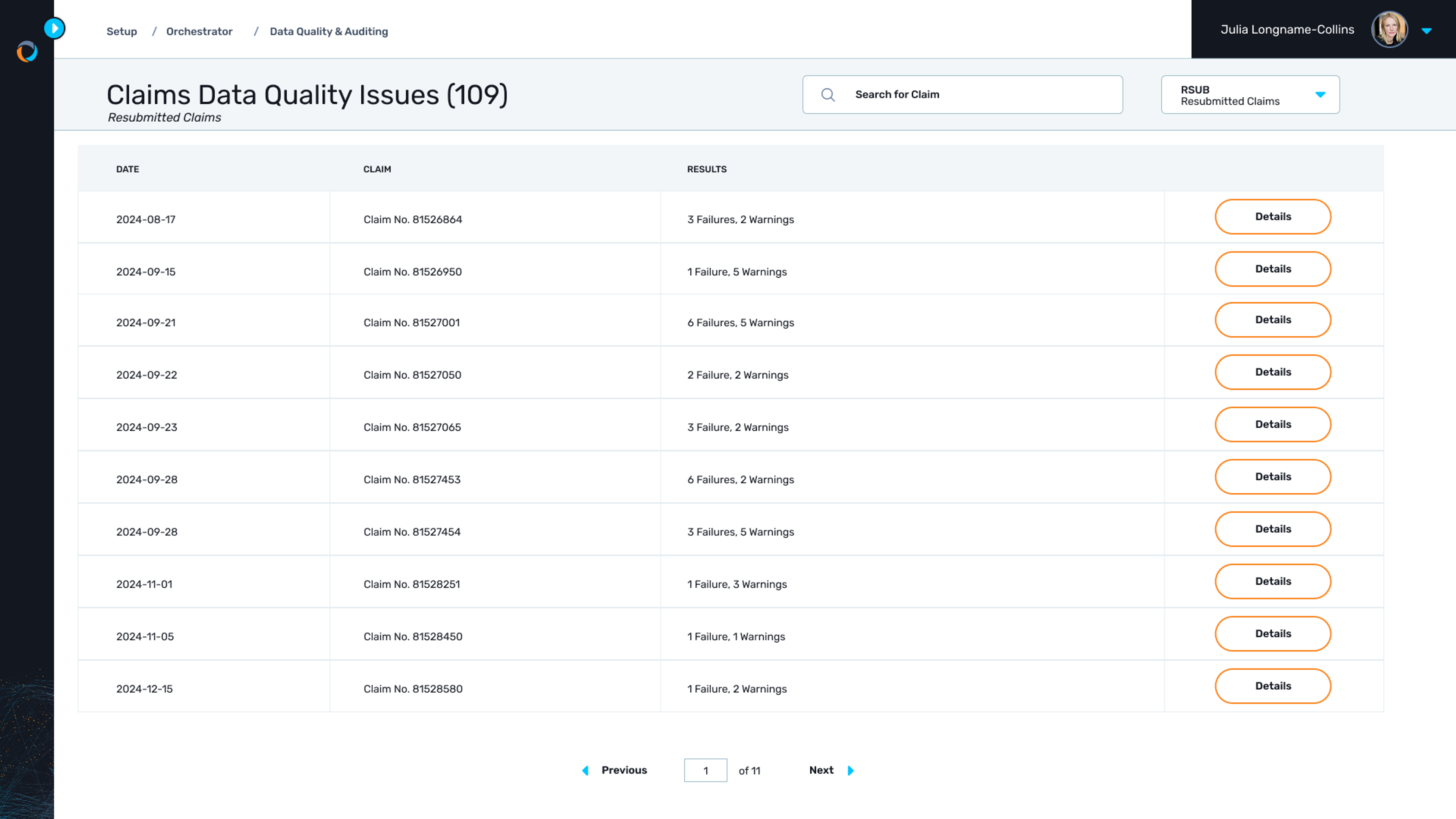
Ensure data accuracy
Automatically identify and resolve errors, inconsistencies, and duplicates in claims data with Gaine's data quality tools.
Unlock data insights
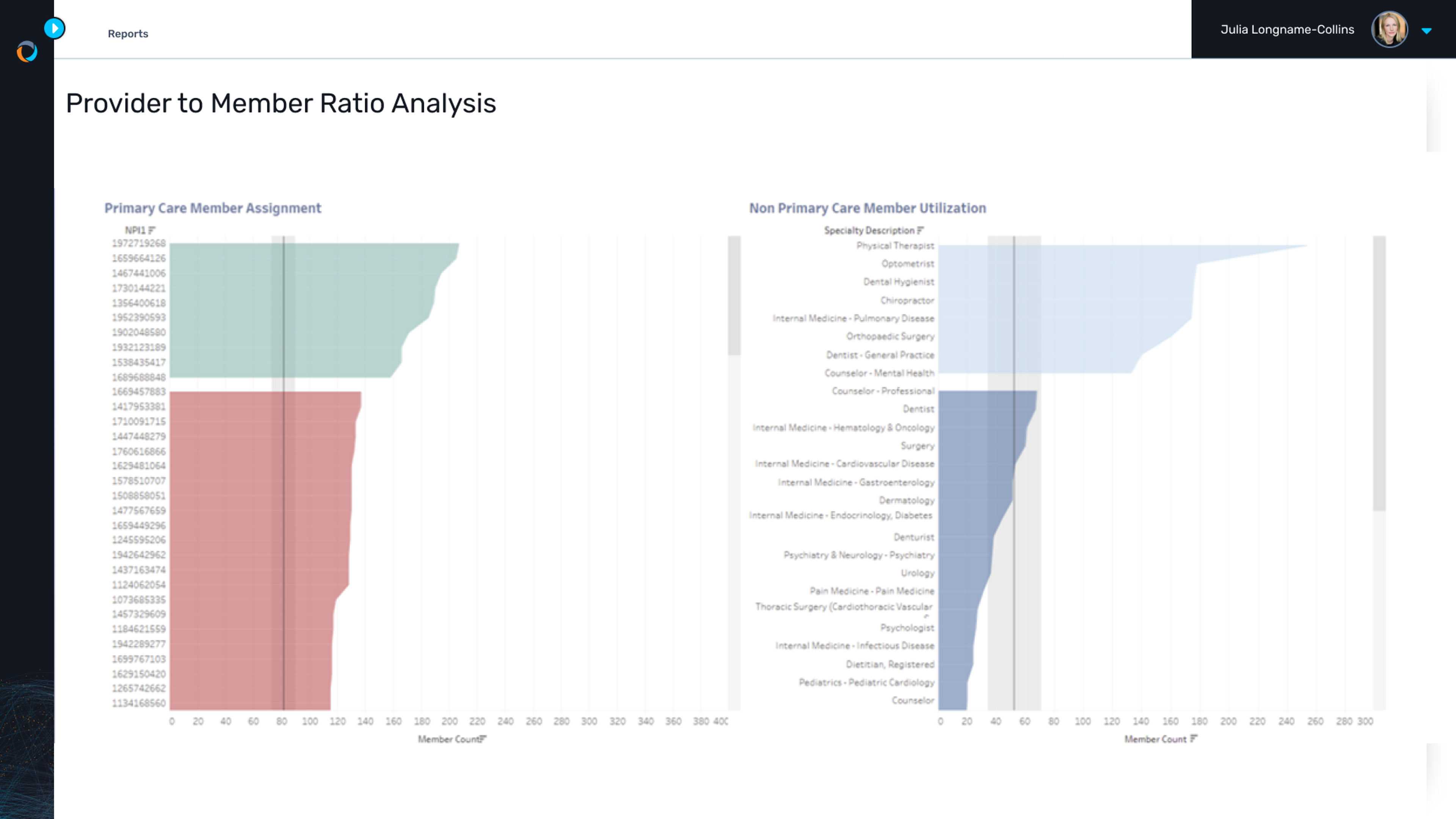
Gain(e) insights into claims trends, cost drivers, and provider performance with the platform's advanced analytics and reporting tools.
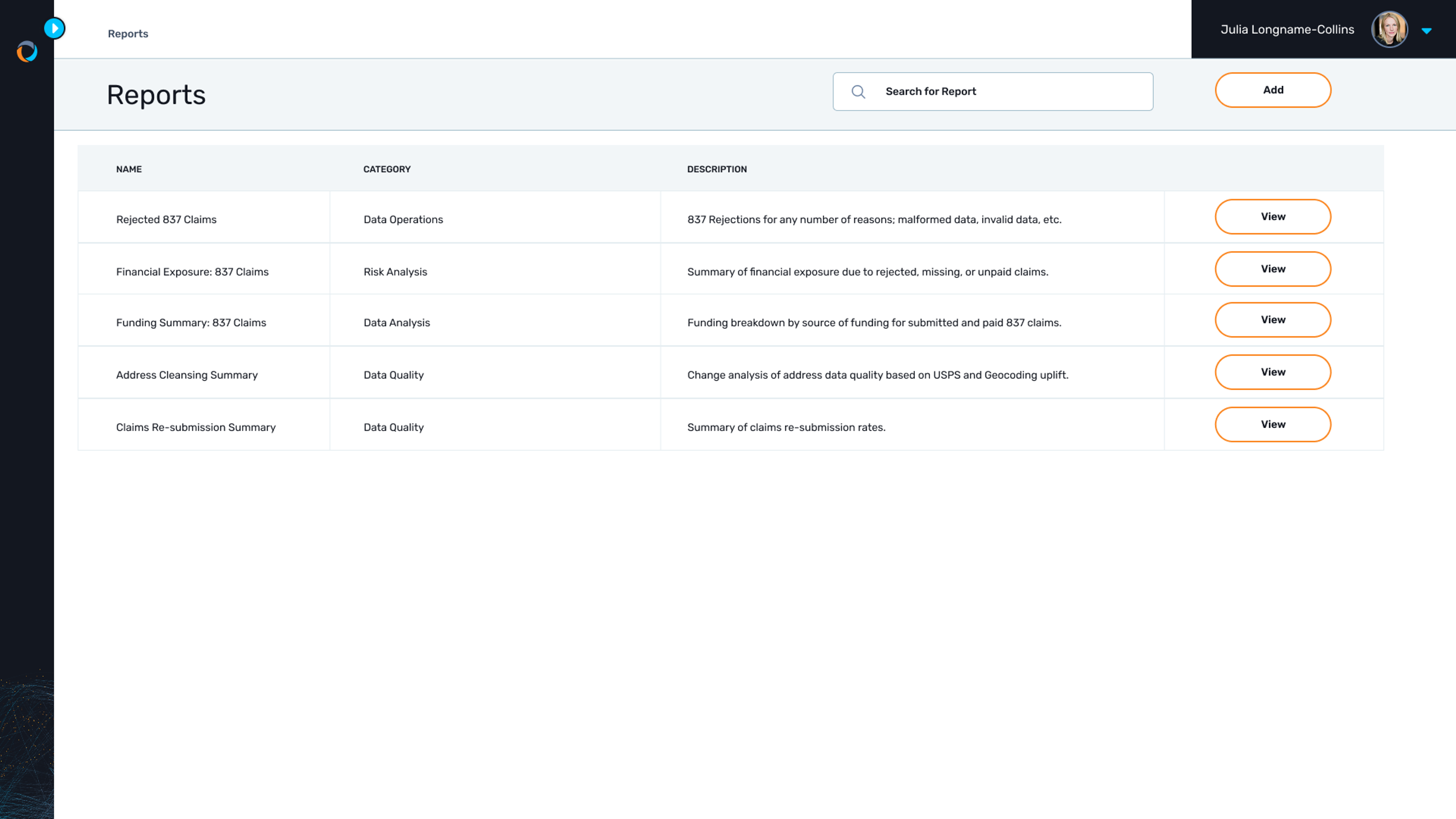
Generate custom reports
Create custom reports tailored to your specific needs, providing valuable insights into claims performance and trends.
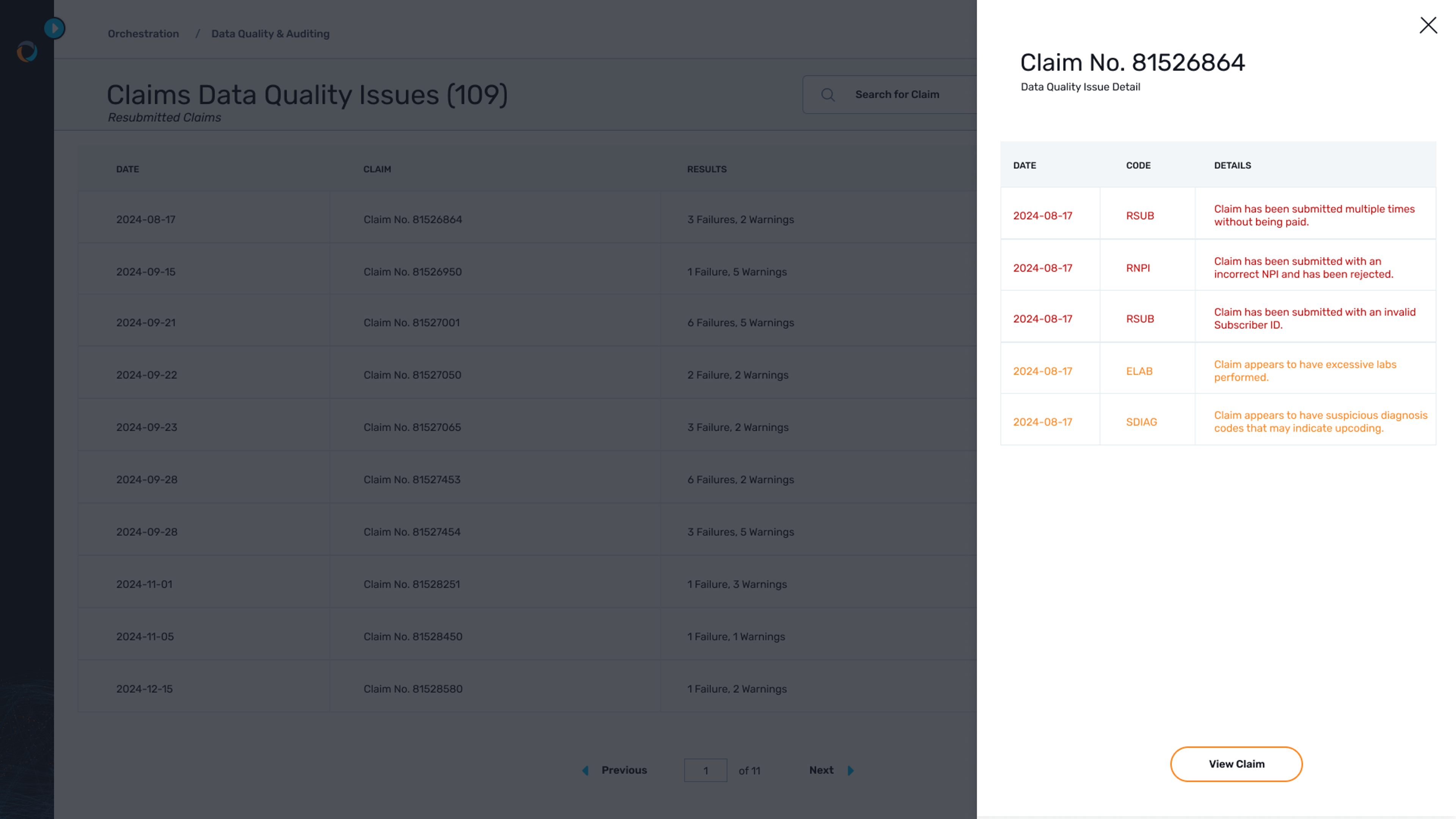
Knock down fraud, waste, and abuse
Conduct comprehensive fraud, waste, and abuse audits with Gaine's advanced analytics and anomaly detection capabilities.
Share data with providers
Securely share claims data with providers to facilitate collaboration, resolve discrepancies, and improve network performance.








