blog
What’s Possible with Health Plan Data Analytics
SECTIONS
The healthcare industry—like every other part of the business world—is now run by big data. For health plan providers, this can be either an asset or a source of overwhelm, depending on their ability to manage data and leverage it strategically. Health plan data analytics is the key to doing this successfully.
With a health plan data analytics strategy in place, organizations can get a handle on the massive volume of data generated by members and providers every day, then use it to make smart decisions and optimize services, strategies, and revenue opportunities.
In this guide, we’ll cover what you need to know about health plan data analytics, how to implement it effectively, and the tools and processes you need in place for it to succeed.
Key Takeaways:
- Health plan data analytics deliver deep insights at the macro, market, organization, customer segment, and individual member levels.
- It requires data collection across many sources and data types, powered by the use of tech tools like master data management (MDM) platforms.
- Key capabilities enabled by health plan data analytics include: predictive modeling, costs management, personalized member engagement, and quality improvement.
- It’s important to lay the foundation for a solid analytics strategy by taking steps like mapping your data sources, setting goals, and adopting the right software tools.
Health Plan Data Analytics: Overview and Key Use Cases
Health plan data analytics is the process of collecting and analyzing vast amounts of healthcare data to extract insights and optimize health insurance plans. It leverages artificial intelligence (AI) technology and statistics to gain a deep understanding of healthcare trends, patient behavior, and cost drivers.
Key components of health plan data analytics include:
Diverse Data Collection
Health plans gather data from a diverse set of sources, including claims records, electronic health records (EHRs), mobile devices and wearables, and member or provider portals (among others). This data can be structured or unstructured and may encompass clinical, financial, and administrative information.

Image Source: http://primedatacenters.com
Data Analysis
Sophisticated analytics tools and algorithms are used to process and analyze the collected data. This involves identifying patterns, trends, and outliers to gain insights into factors like healthcare utilization, disease prevalence, and treatment outcomes.
Today, data analytics software is essential to handle the massive volume of data now processed by health insurance and healthcare providers, and to leverage AI and other advanced capabilities.
Predictive Modeling
Health plan data analytics also involves predictive modeling to forecast future healthcare costs, identify high-risk individuals, and tailor interventions to prevent costly health issues. This forward-thinking aspect of the process is critical as our technology-driven world moves faster, member expectations evolve, and changing trends demand greater agility from healthcare organizations.
Cost Management
By understanding the drivers of healthcare costs, health plan providers can make informed decisions about pricing, reimbursement rates, and cost containment strategies. This both drives greater revenue for organizations and enables better resource allocation to enhance member services.
Personalized Member Engagement
Personalization is a core part of modern member engagement for health insurance providers. In fact, it’s both a standard member expectation and a huge opportunity for competitive advantage. Today, 75% of patientsOpens in a new tab say they want deeper personalization from healthcare and health plan providers—but only 54% think providers are doing a good job of it.
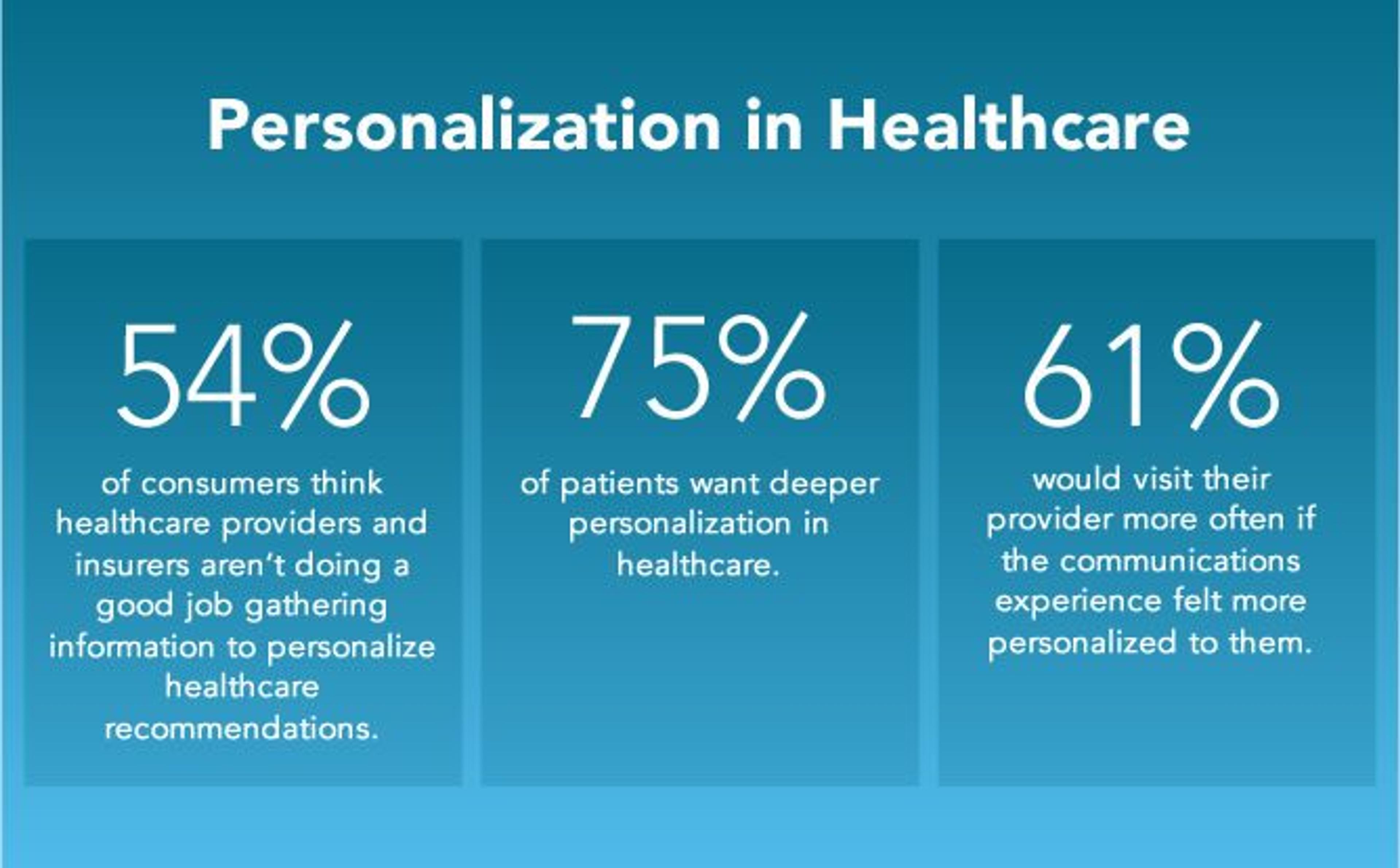
Image Source: https://www.idomoo.com/blog/personalization-in-health-and-wellness-top-6-digital-trends/
Health plan data analytics uplevels an organization’s ability to personalize health plans and tailor features and benefits to individual member needs. As a result, members receive better-quality benefits and care, and health plan providers are able to win new customers over competitors not offering the same level of personalized service.
Quality Improvement
Data analytics can also aid in assessing key performance indicators around the quality of care delivered to members and identifying areas for improvement. This enables health insurance providers to meet changing member preferences and needs, continually improve the services and benefits they offer, and remain accountable for meeting internal expectations and goals.
Laying the Foundation for Health Plan Data Analytics
The volume and scope of healthcare data today requires that organizations lay a strong foundation for implementing their health plan data analytics strategy. Doing so requires a few important steps:
1. Map Your Data
Begin by comprehensively mapping your data landscape. Identify all sources of data and how it flows in and out of your organization. Identify and document key data privacy and compliance considerations relevant to your organizations. This step ensures that no valuable data goes overlooked, all data is being handled properly, and you’re able to set up efficient data pipelines.
2. Adopt an MDM Tool
Master Data Management (MDM) is an indispensable part of health plan data analytics that ensures the standardization, uniformity, accuracy, and consistency of your data. It’s enabled by adopting an MDM software solution, which allows you to centralize and manage large volumes of data, scale your strategy, and automate much of the process.
3. Set Defined Goals
Every healthcare organization has its own unique mission, member and customer bases, needs, goals, capabilities, and operating structure. It’s important to clearly articulate your objectives for health plan data analytics and how they fit with the unique aspects of your organization.
Define your goals using a documentable framework (like SMART goals, shown below) to ensure your health plan data analytics strategy has clear metrics you can use to measure progress and effectiveness, and is designed to drive real outcomes and results.
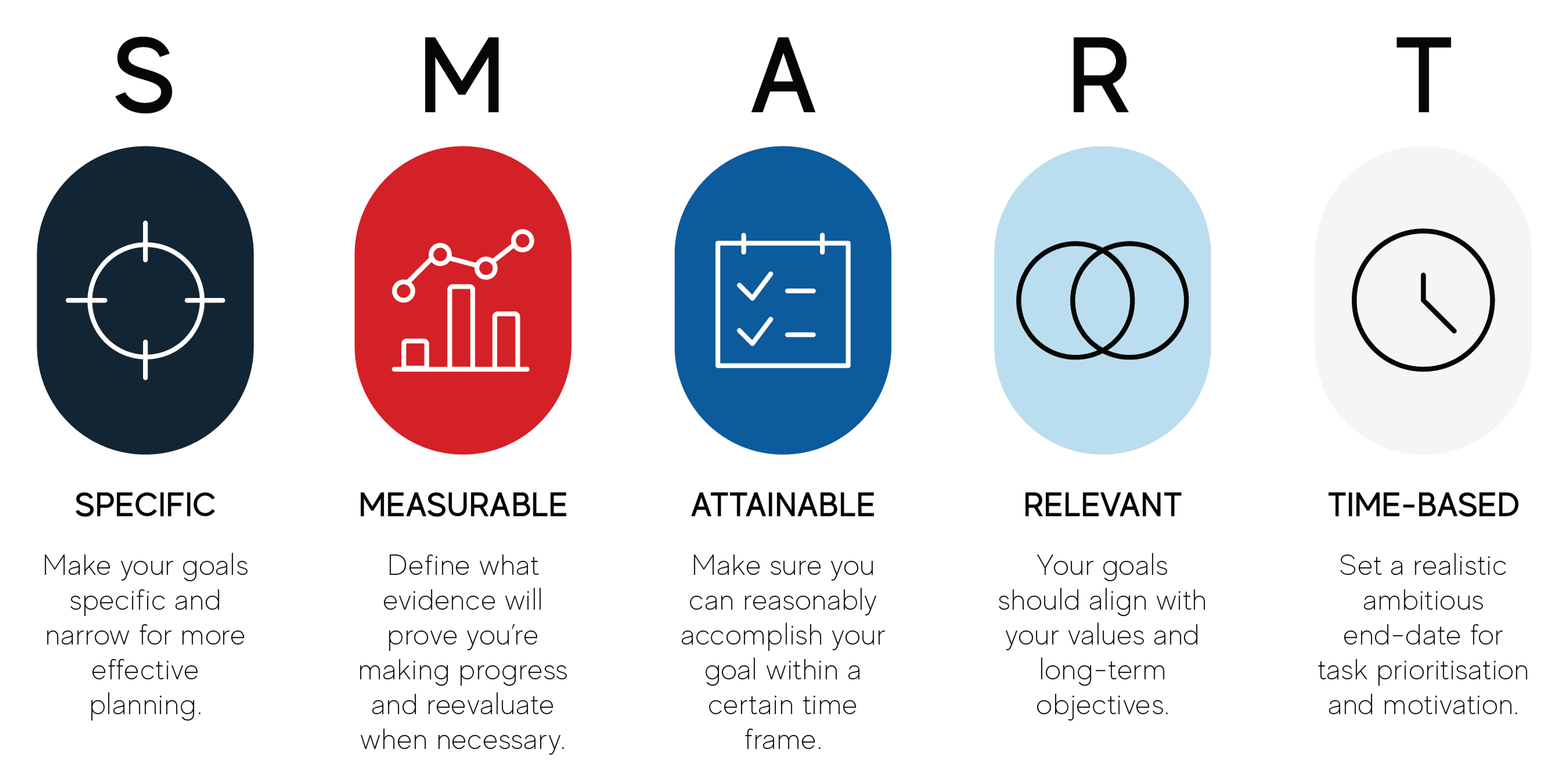
Image Source: https://www.futurelearn.com
Whether it’s reducing costs, improving member satisfaction, or enhancing care quality (or something else), having well-defined goals ensures that your analytics efforts remain focused and aligned with your organization’s strategic priorities.
4. Train Employees
Equip your employees with the necessary skills and knowledge to leverage data analytics effectively. Offer training programs and workshops to build analytical capabilities at your organization. Data literacy among your workforce is key to unlocking the full potential of your health plan analytics strategy.
5. Monitor, Refine, Adjust
Establish a continuous monitoring and improvement process for health plan analytics. Regularly assess the performance of your analytics initiatives, refine your models and strategies, and be agile in adjusting your approach as new data sources and technologies become available.
Putting it All Together
Health plan data analytics is not just a nice-to-have for healthcare organizations in today’s fast-changing and technology-driven landscape—it’s a must. Having an analytics strategy allows you to stay on top of changing trends, track and analyze performance, understand customers, find opportunities to improve, and stay more agile.
Putting the right tools and processes in place is the first step toward implementing a strategy designed to succeed, and an MDM platform is one key tool every organization should include.
MDM ensures your organization can maintain a single, standardized source of data truth, analyze data in a centralized location, access real-time updates, and effectively collaborate and share insights.
Gaine’s Coperer platform is a scalable, ecosystem-wide MDM solution specifically designed for the unique challenges of the healthcare and life sciences industries. Contact us to learn more about how Coperer can help you transform your data capabilities.
