Understanding the Provider Data Management Lifecycle
Understand the limitations of traditional provider data management and what to look for in a modern provider data management solution.
Coperor’s Provider Data Management solution empowers payers to maintain accurate, up-to-date, and compliant provider information, improving efficiency, reducing costs, and enhancing both provider and patient experiences.

Healthcare payers face significant challenges in maintaining accurate provider data within a dynamic ecosystem. Coperor addresses this complexity by maintaining a consolidated view of providers across credentialing, contracting, network management, and directory systems. This comprehensive approach enhances data accuracy and operational efficiency, ultimately improving both provider and patient experiences.
VP of Operations, Texas-based health insurance provider
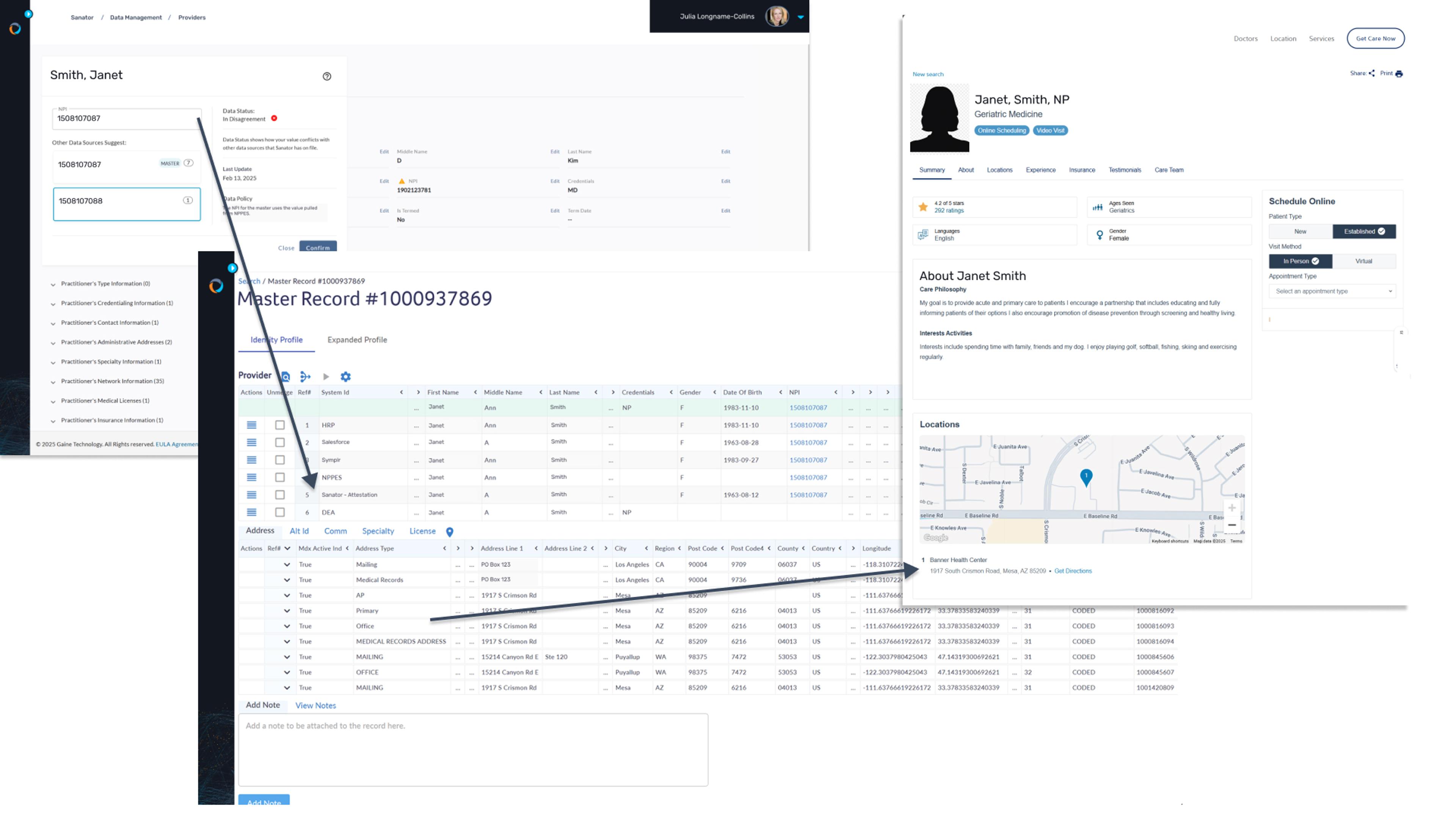
Coperor HDMP provides a centralized platform for managing provider data, allowing you to update data once and then automatically distribute it across all connected systems. This approach ensures that each application receives consistent, high-quality data without requiring separate data management in each point solution. By centralizing data management, you can reduce administrative burdens, enhance data consistency, and improve operational efficiency.
Streamline your data assets efficiently
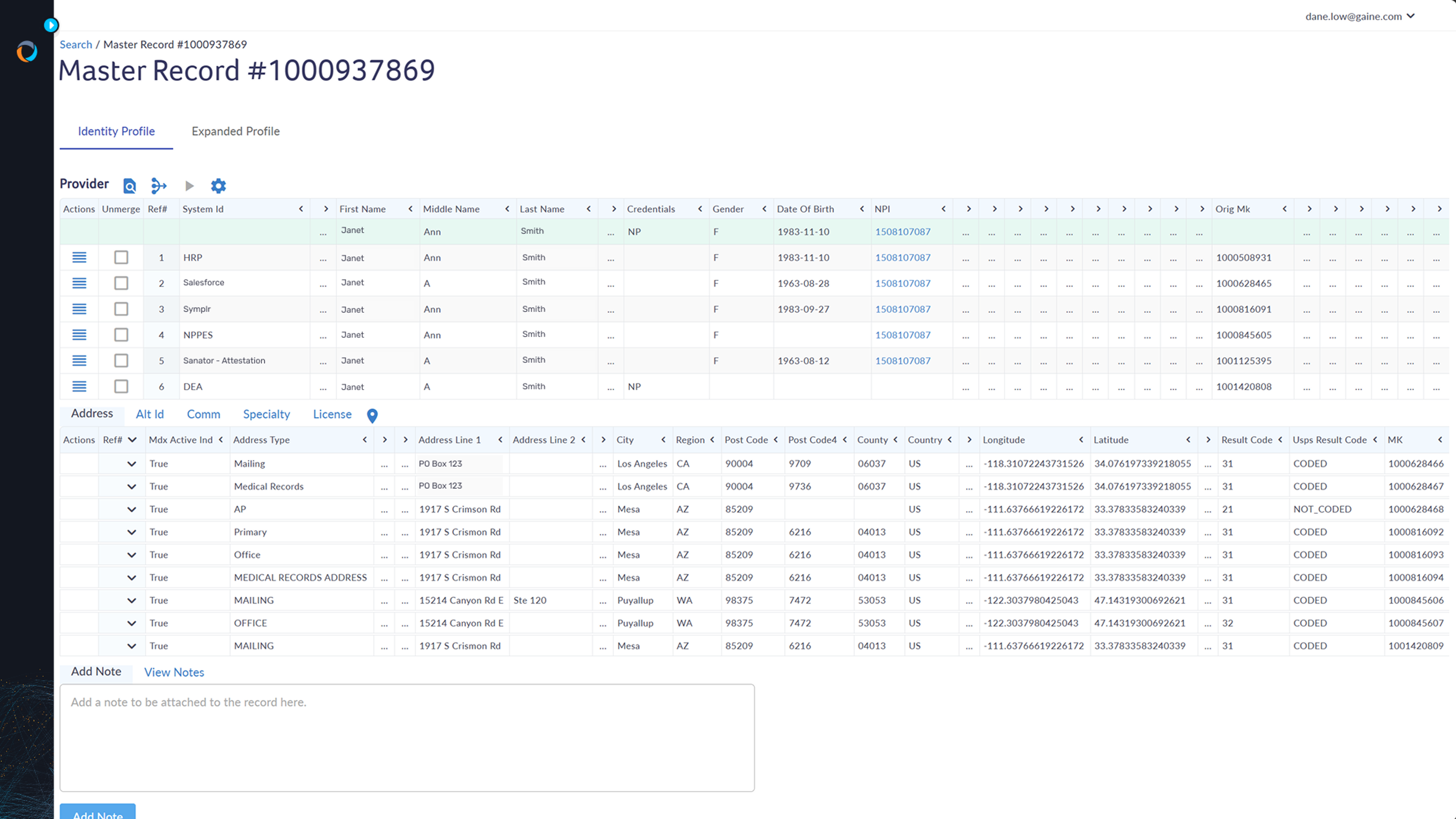
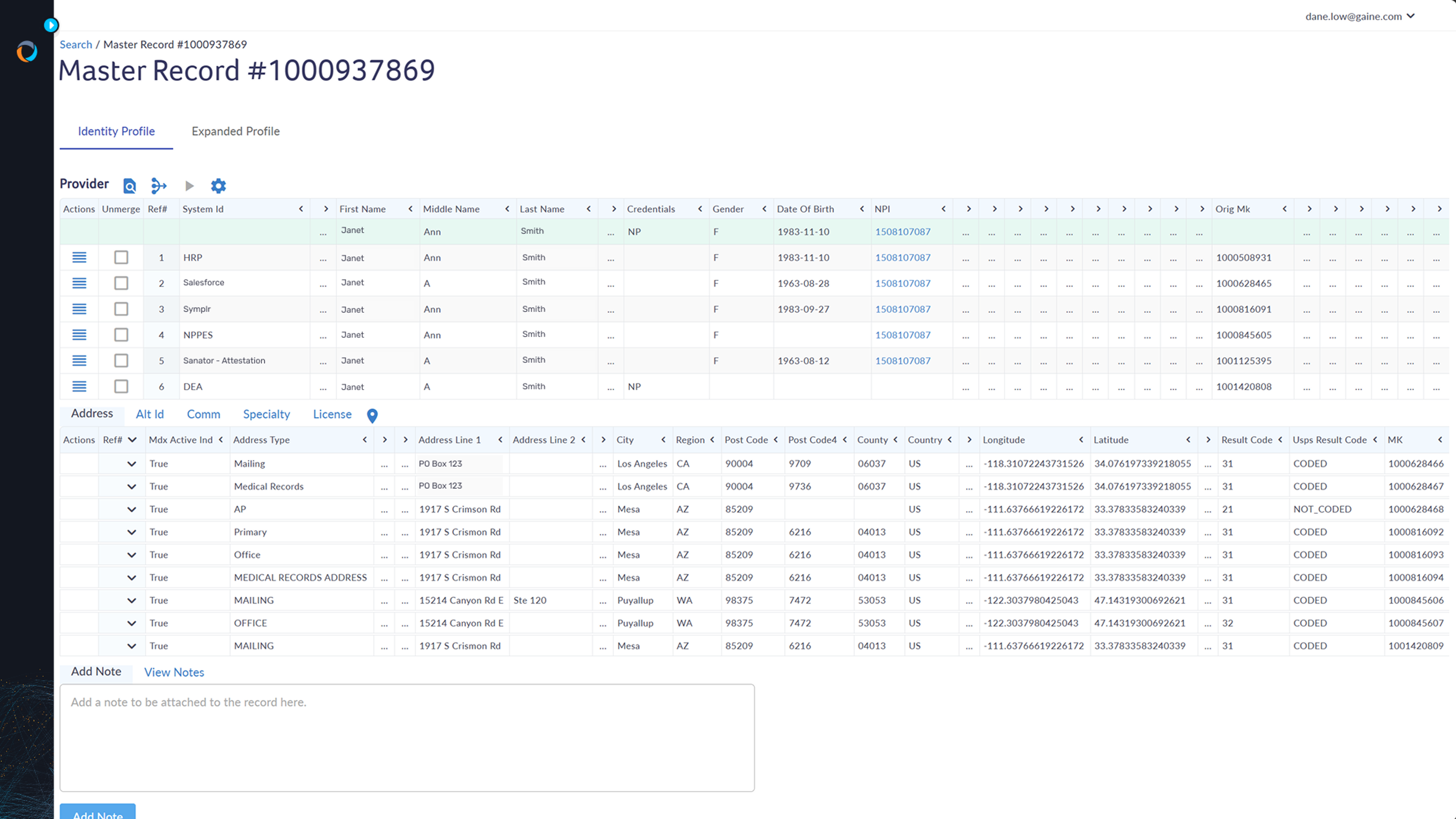
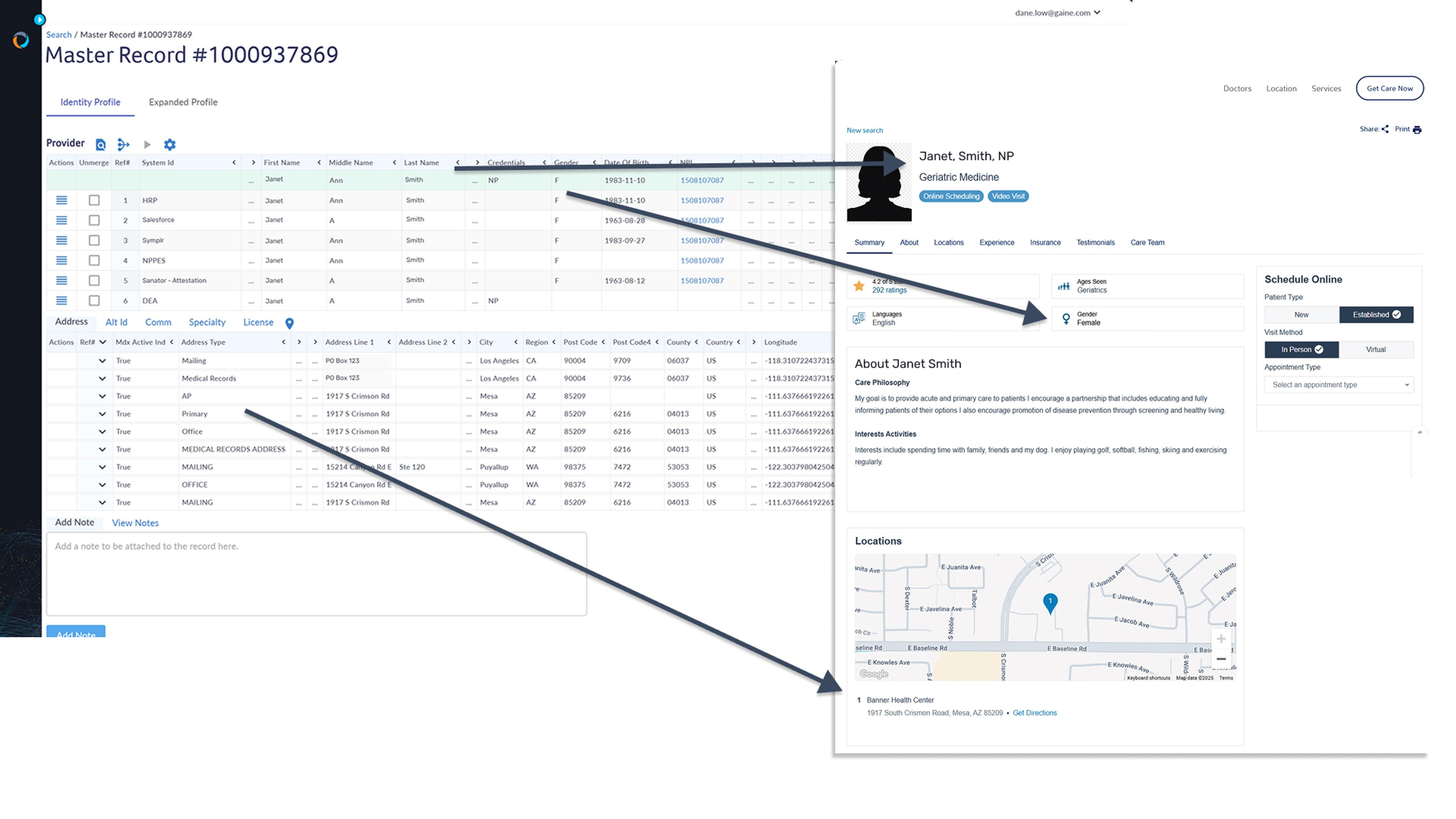
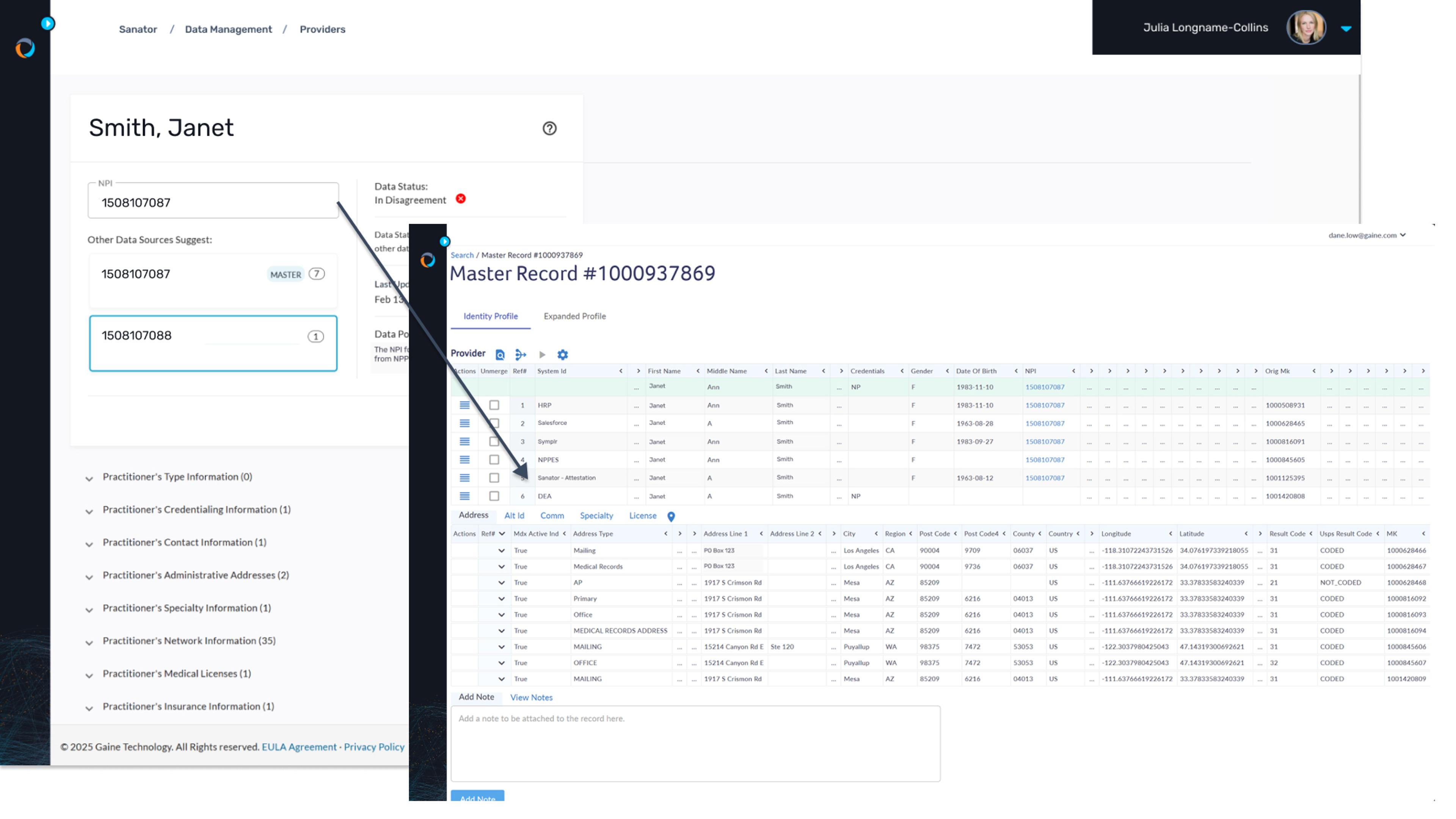
Coperor HDMP offers enterprise-grade master data management, validating and enriching provider data with internal and reference sources like NPPES and DEA. This ensures accurate, consistent data across all systems, reducing errors and discrepancies. It maintains golden records with rules to reconcile discrepancies, ensuring up-to-date provider information.
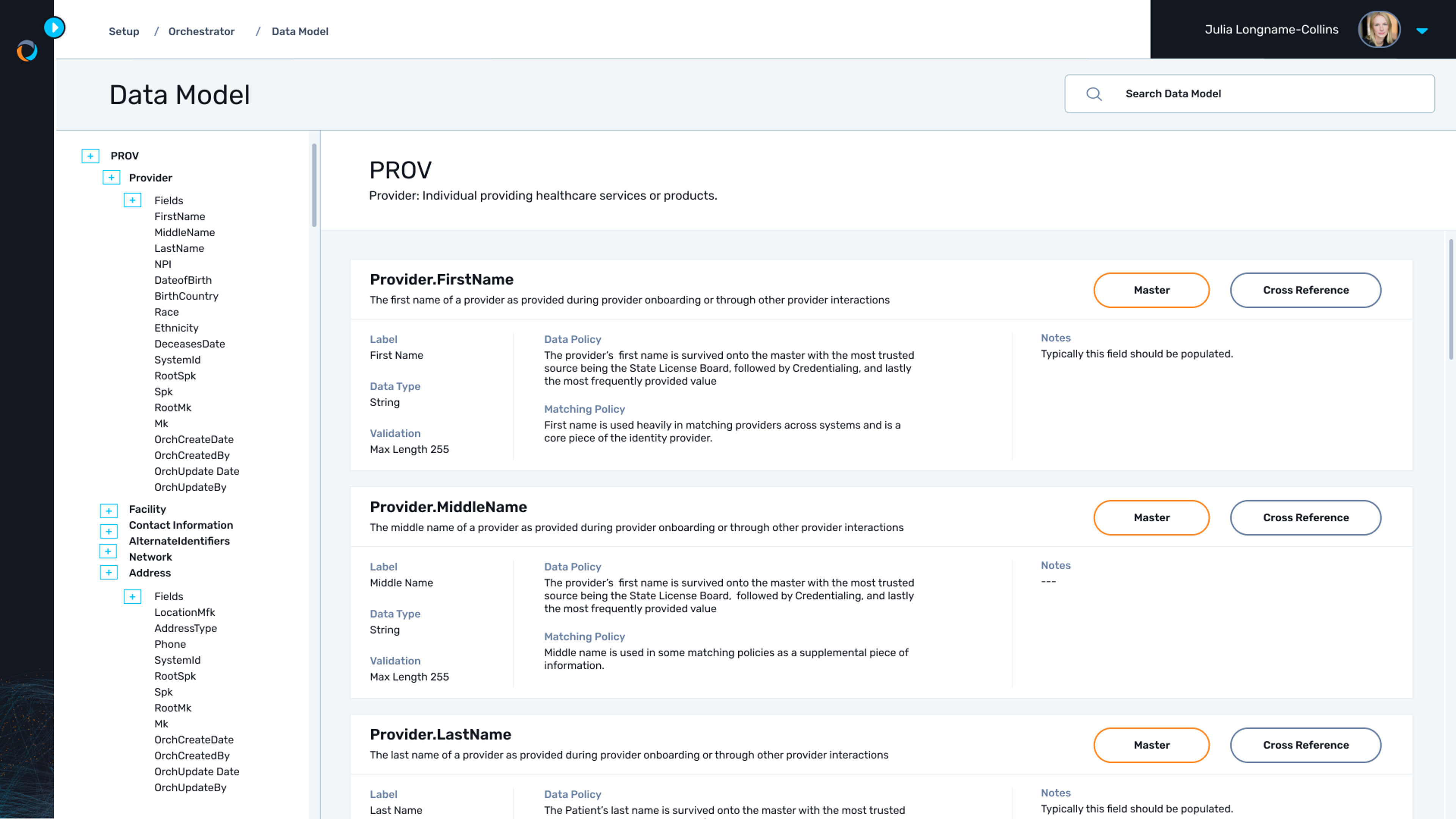
Benefit from a proven framework
Leverage Gaine Coperor's pre-configured data model, specifically designed for healthcare and battle-tested and refined through 15 years of experience implementing HDMP across leading healthcare organizations. The model and out-of-the-box business rules ensure that key considerations are addressed and potential issues are mitigated, allowing for faster deployment and reduced risk.
Adapt data to any format needed
Coperor HDMP transforms provider data into any format or structure needed for the systems you need to distribute it to, without compromising your source of truth. This capability saves you time and effort by automatically formatting data for each application, eliminating the need for manual data wrangling. Additionally, it ensures privacy compliance by providing each system with only the information necessary for its specific needs.
Sync data across systems in real-time
Instead of simply moving data from System A to System B, C, D, and Z, Coperor keeps all your healthcare data, systems, and applications connected in lock-step. Coperor HDMP synchronizes provider data in real-time across all connected systems, ensuring that updates are immediately reflected everywhere. This real-time synchronization prevents data conflicts and ensures that all stakeholders have access to the most current information, enhancing operational efficiency and decision-making.
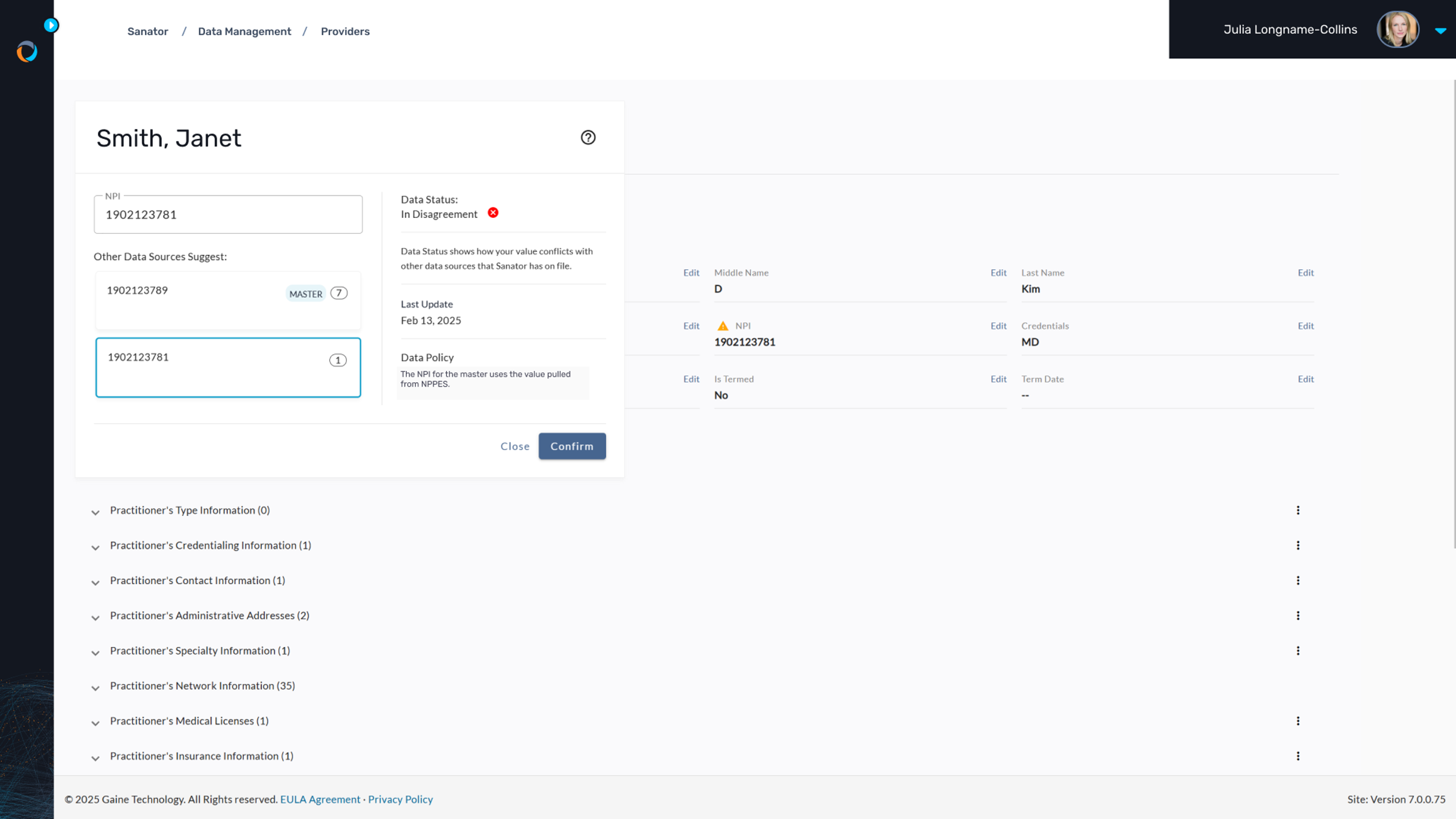
Ensure data integrity always
Coperor HDMP provides robust data governance capabilities, ensuring that provider data is accurate and up-to-date. It resolves discrepancies through automated processes and manual intervention when necessary, maintaining trust in your data and supporting regulatory compliance. This governance is crucial for maintaining high-quality data across all systems.
Automate accurate provider directories
With Coperor, you can maintain accurate and compliant provider directories by ensuring that all provider information is up-to-date and consistent across systems. The platform supports real-time collaboration through a provider portal, allowing providers to easily attest and update their information once, which is then automatically distributed across multiple health plans. This streamlined process enhances data accuracy, reduces administrative burdens, and improves regulatory compliance.