blog
5 Advances in Automated Claims Processing
SECTIONS
Gone are the days of filing medical claims with labyrinths of paperwork, phone calls, and manual tasks. Today, claims process automation has transformed into a process that’s efficient and even focused on providing a real customer experience—one that eliminates pain points like late payments and arduous customer service needs, and builds better relationships between patients and providers.
At the center of automated claims processing are artificial intelligence and data analytics technologies, powering advancements in a wide range of areas. This article will explore 5 important advancements on the forefront in 2024, and the impact they’re making in the larger healthcare insurance landscape.
Key Takeaways:
- Claims process automation uses a combination of AI, ML, data analytics (and other) technologies to make the claims process more efficient, reduce risk, and improve accuracy.
- Platform-based software tools are transforming the process by eliminating silos and centralizing data in one place.
- Increased use of electronic health records (EHRs) is making claims processing more accurate by providing more comprehensive medical histories.
- Collaboration between key players like providers, payers, and vendors is crucial for effective claims processing.
- Development of mobile-native technologies has become essential for aligning the claims process with user preferences and behaviors.
What is Claims Process Automation?
Claims process automation means using modern technologies to streamline and automate the process of filing medical claims. Once a notoriously manual and time-consuming process, claims process automation makes it more efficient while reducing the need for human intervention (and thus human error).
As you can see in the flowchart below, manual claims processing includes many separate steps that create silos between the people involved. Automated claims processing, on the other hand, involves an automated data flow that connects the dots between every step of the claims process.
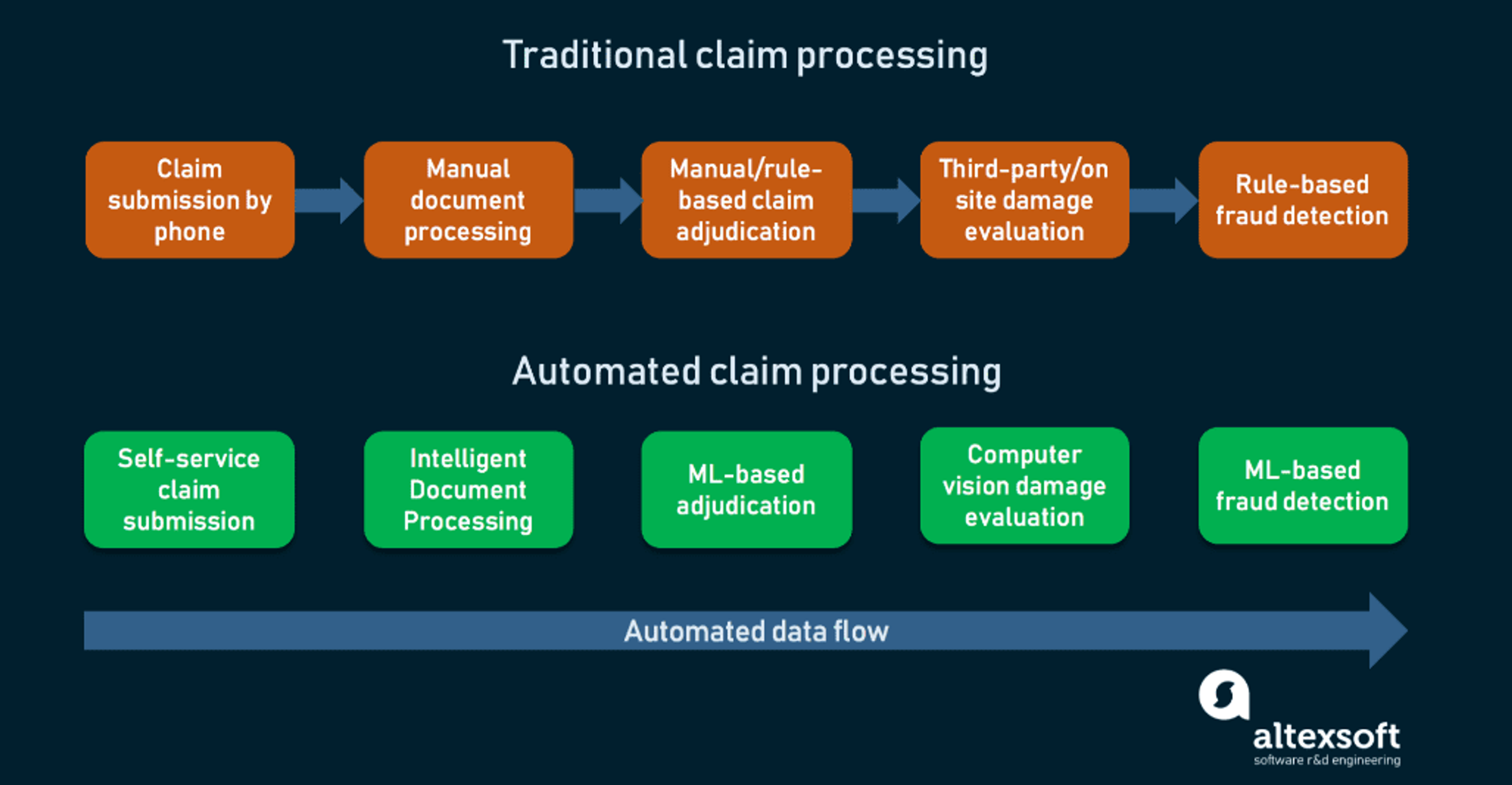
Image Source
The backbone of automated claims processing systems is the combination of advanced technologies like artificial intelligence (AI), machine learning (ML), and data analytics.
AI and ML interpret and process complex claims data, identify anomalies, and predict potential issues before they even arise. Machine learning in particular is crucial for adapting to new scenarios and making claims processing more efficient with each iteration.
At the same time, data analytics provides deep insights that help organizations understand trends, detect fraud, and make informed decisions. Analytics software solutions ensure data is accurate, consistent, and easily accessible to those who need it, while keeping it secure and compliant with data privacy laws.
These technologies are also always evolving, and thus the claims process is enhanced by new capabilities all the time. Let’s look at 5 specific advances in automated claims processing happening in 2024.
5 Advances in Automated Claims Processing
Centralized, Platform-Based Claims Processing
Automated claims processing would be impossible without comprehensive software systems to support the process. Modern platform-based claims processing software solutions streamline tasks at every stage of the process, including claim intake, data gathering, analysis, and final decision (among others).
They’re also designed to assess the risk of each claim that comes through, identifying complex cases and potential fraud. They ensure that all claims are complete, accurate, and compliant with established coding standards, thereby reducing the administrative burden on human employees and enhancing the efficiency of the claims process.
Health Information Technology
Health information technology (IT) systems, such as electronic health records (EHRs) and personal health records (PHRs) have become integral to modern claims processing. As they become more prevalent in the world of healthcare, gradually replacing paper health records completely at most organizations, it is becoming easier to automate the claims process.
EHRs, for example, give players across the claims process access to more comprehensive patient medical histories, allowing claims processing software to accurately analyze the medical necessity of each claim.
Health Information Exchange (HIE) platforms facilitate seamless data sharing between payers and providers, ensuring all parties have the information needed to make the right decision without the need for multiple phone calls or other back-and-forth communication.
Today, 96% of healthcare providersOpens in a new tab use EHRs, meaning they’re fast-becoming a ubiquitous resource for more accurate, informed, automated claims processing.
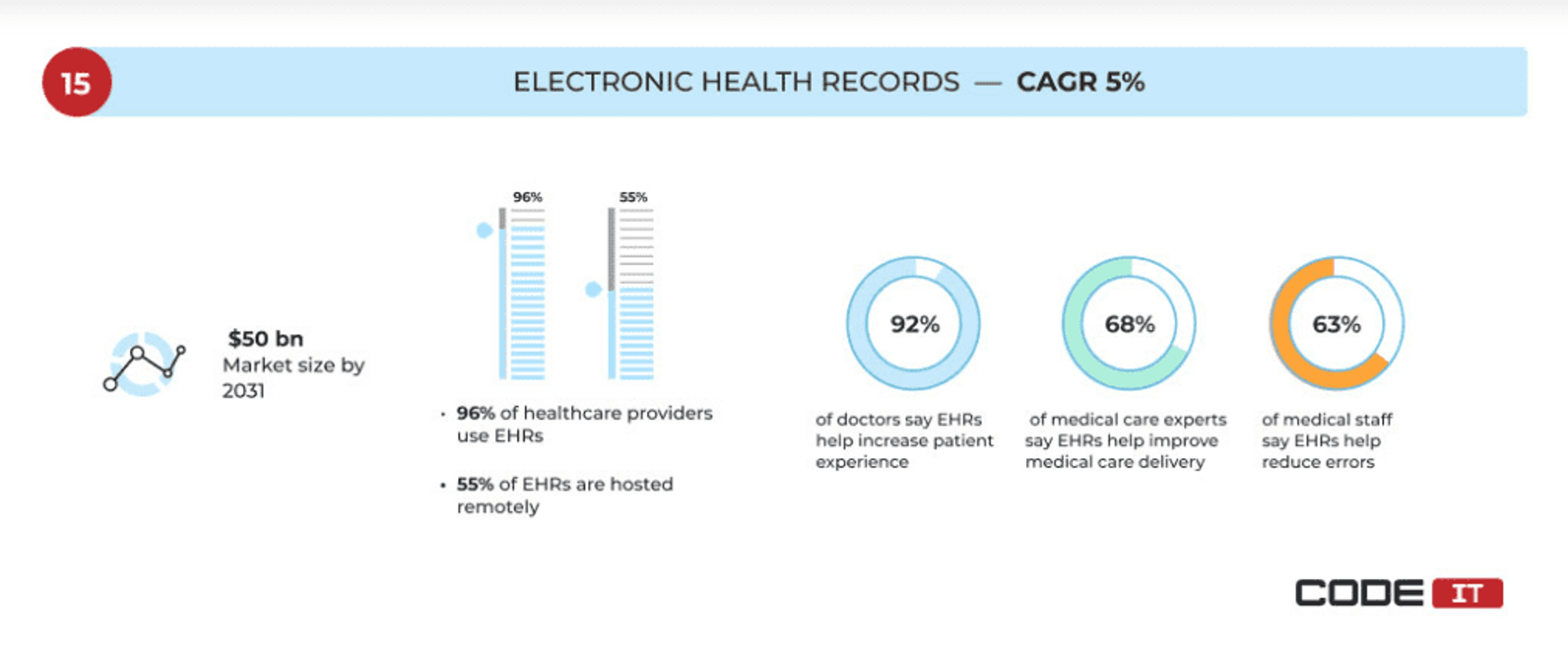
Image Source
Intelligent Document Processing
The industry shift toward EHRs has one complicating factor: Decades of paper-based patient records that already exist. These records need to be converted to electronic format in a way that allows automated claims processing software to actually extract the information they contain. Intelligent data processing (IDP) is an AI-powered capability that makes this possible.
Rather than just transferring documents into electronic systems as images, IDP can extract data from structured, semi-structured, and unstructured documents to be processed further by data analytics and AI-based software tools. They can then save the documents in various formats that can be edited and manipulated, like CSV or excel.
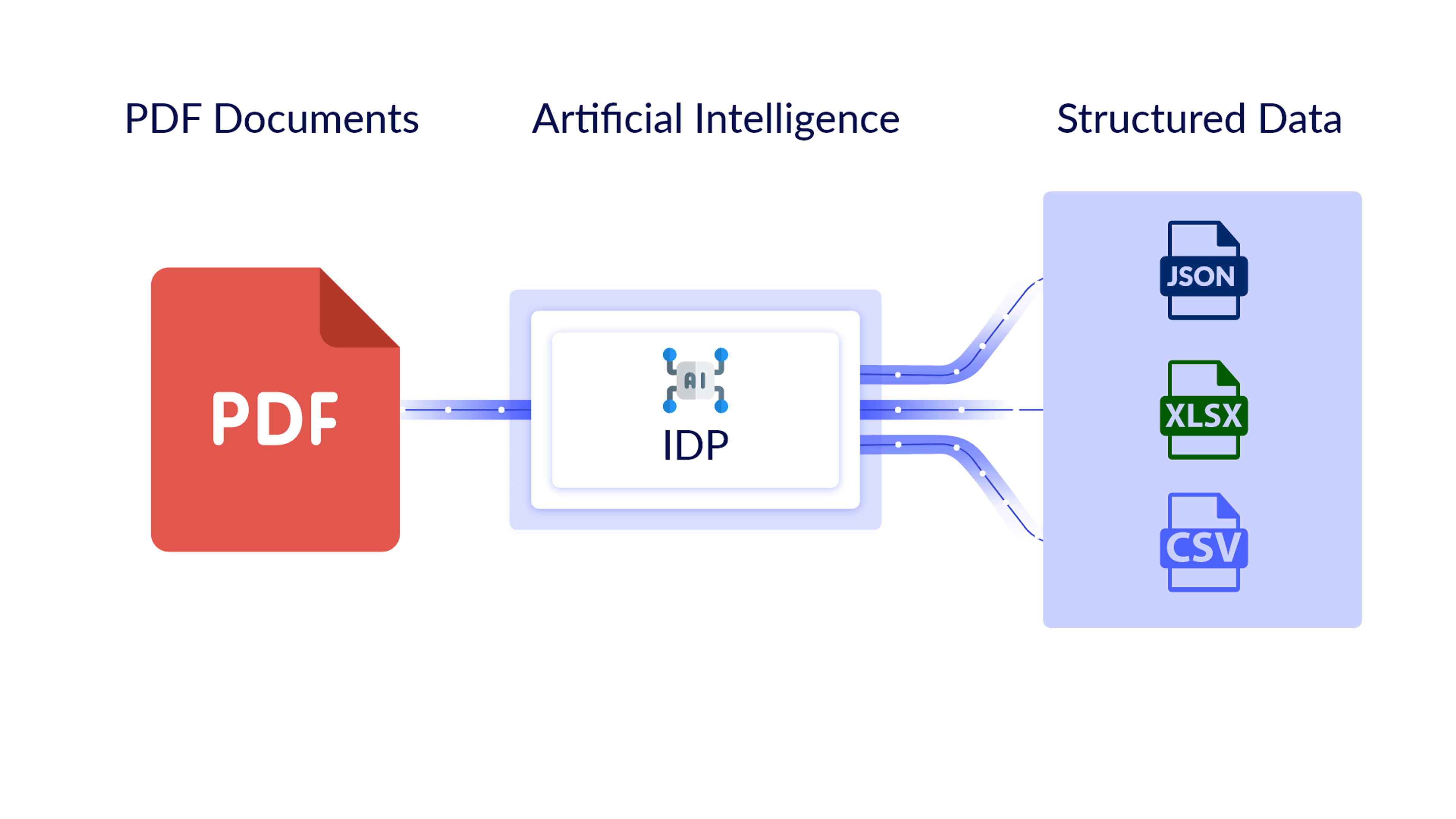
Image Source
This makes it possible for claims process software to more effectively analyze medical history data from previous records and make more informed decisions.
Vendor Partnerships for Claims Management
Modern technology makes it possible for players across the healthcare ecosystem to collaborate more effectively, integrating specialized solutions with an organization’s core systems. Claims processing is one area where this collaboration has a significant impact.
Specialized vendors in areas such as billing, payment processing, and claims management make the backend processes involved with claims processing smooth and efficient, while also enhancing the user experience during steps like claim submission or customer service inquiries.
Automation is involved at every turn, from claims analysis, to AI chatbots that respond to customers in real time, to automated reminders to keep the process moving when information is missing.
Mobile-Native Claims Solutions
People now use their smartphones to complete tasks in every area of their lives, and healthcare is no exception. As such, the development of mobile-native healthcare technology has been critical to making progress in automated claims processing and enhancing the user experience throughout.
Mobile apps and platforms enable users to conveniently complete steps like submitting claims, tracking claim status, and making payments, speeding up time to resolution. At the same time, they deliver users real-time updates right on their phone, reducing the need for frequent customer service calls.
Market demand for these types of apps has been on the rise for nearly a decade, and is projected to keep growing over the next several years, emphasizing the central role they’ll continue to play.
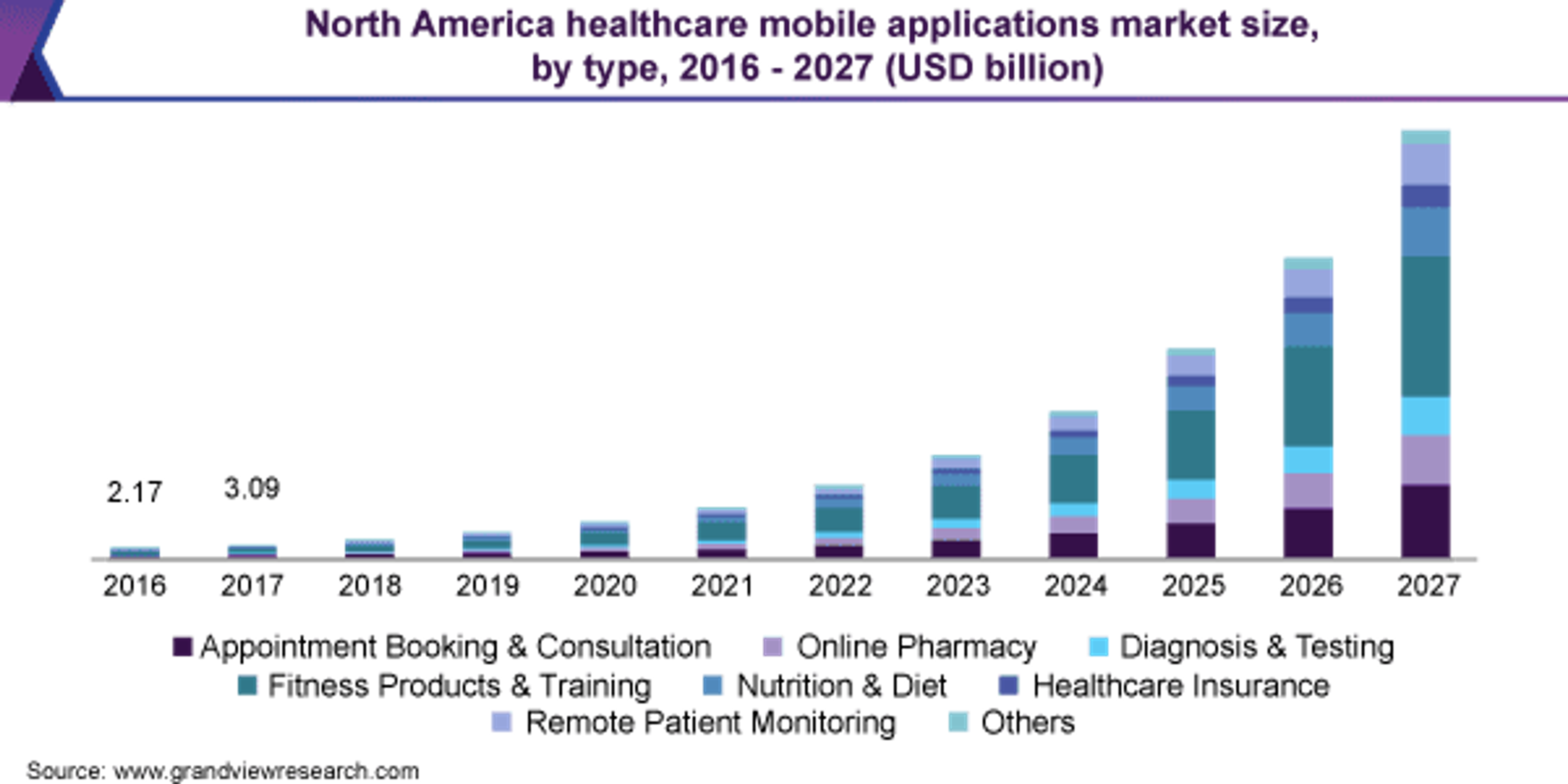
Image Source
Looking Ahead
Automated claims processing is an essential capability for organizations operating in today’s fast-paced and data-driven healthcare landscape. Not only is it streamlining internal processes for better efficiency, it’s also contributing to better customer experiences (and thus relationships) at the same time.
As technologies like AI, ML, and data analytics keep advancing, we’ll undoubtedly see the capabilities mentioned above become more sophisticated, while new ones continually emerge. To keep up, organizations must adopt solutions that are comprehensive and can be integrated with their existing systems (and those of their partners).
Gaine’s Coperer platform is an ecosystem-wide software solution designed specifically for the unique challenges and needs of healthcare organizations. Start your real-time Coperer demo to learn more about how we can help you transform.
